Session Information
Date: Saturday, November 16, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Vascular Ultrasound (VUS) performs well in diagnosing Giant Cell Arteritis (GCA) but its role in monitoring disease activity and in predicting outcomes is unknown (1). Different quantification scores have been proposed for VUS in GCA but their precise role in routine clinical practice has yet to be established (2). Published values for Intima-Media Thickness (IMT) exist which can identify vascular inflammation but require validation (3). This study evaluates the Halo Count (HC), Halo Score (HS) and OMERACT GCA US Score (OGUS) in a prospective GCA cohort and defines their diagnostic and prognostic value. It aims to compare the performance of VUS scores with all other patient variables for GCA diagnosis and prognostication. This study also evaluates the optimal IMT cut-off points that define the presence of vasculitis on US.
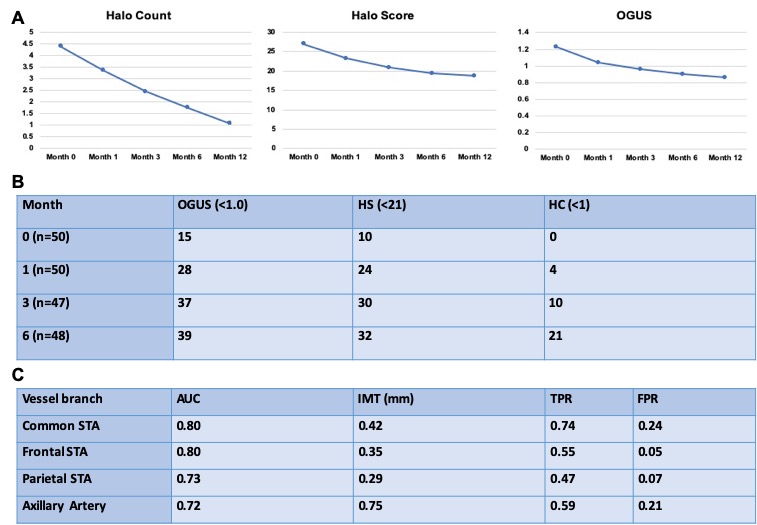
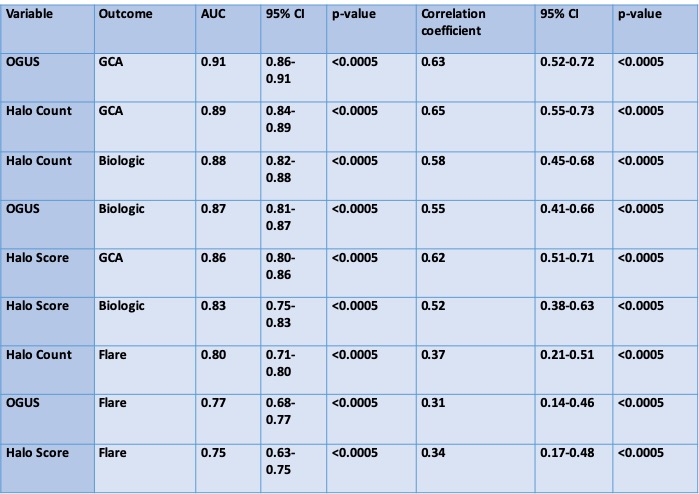
Methods: 57 newly diagnosed GCA patients (clinical diagnosis confirmed by two rheumatologists) were recruited. VUS (of Superficial Temporal and Axillary Arteries) were performed at baseline and again at 1, 3, 6 and 12 months. AUC analysis was used to define the optimal IMT cut-off point for each branch of STA and AA that correctly identified the presence of vasculitis. Mean VUS quantification scores were calculated at each timepoint and the significance of longitudinal trends were interrogated with Wald tests. Time-to-normalization of scores were evaluated with abnormal thresholds as follows; HC ³1, HS ³21, OGUS ³1.0. Correlation coefficients and AUC analysis were used to identify which clinical and biochemical variables predict higher baseline VUS scores and to determine which clinical, biochemical and VUS parameters are most predictive of GCA diagnosis, GCA flare, future biologic requirement and future ischaemic complications.
Results: 48 patients had 6 month follow up and 27 patients had 12 month follow up. Mean VUS scores all declined significantly over 12 months (Fig 1A). Of 48 patients, HC, HS and OGUS normalized in 21, 32 and 39 patients respectively by 6 months but no association was seen with adverse events (Fig 1B). The optimal IMT cut-offs for diagnosing GCA in our cohort are outlined in Fig 1C and no significant difference was observed between groups with and without cardiovascular risk factors. Fulfilling 2022 ACR/EULAR Classification Criteria showed moderate correlation with baseline HC, HS and OGUS with higher classification criteria scores showing strong correlation with higher VUS outcome scores. HC, HS and OGUS were superior to all clinical and laboratory parameters predicting future adverse events (Table 1). Incidence of ischaemic events were too low to determine significance.
Conclusion: Quantifying degrees of inflammation on VUS has both diagnostic and prognostic value in GCA as does serial scoring during follow-up. Higher baseline VUS outcome scores were associated with a higher likelihood of GCA diagnosis, flaring within 12 months and requirement for future biologic therapy. OGUS correlated with other VUS quantification scores but normalized earlier. The optimal IMT cut-off points that define the presence of vasculitis on VUS in this cohort differ from previously published values and further research is required to further clarify this.
To cite this abstract in AMA style:
Kirby C, Flood R, Cowley S, Finlay E, Mullan R, Murphy G, Kane D. Quantitative Vascular US Has Additional Diagnostic and Prognostic Value in GCA [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/quantitative-vascular-us-has-additional-diagnostic-and-prognostic-value-in-gca/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/quantitative-vascular-us-has-additional-diagnostic-and-prognostic-value-in-gca/