Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) frequently complicates the disease course in RA. While forced vital capacity (FVC) from pulmonary function tests (PFTs) is the most common measure used to monitor RA-ILD, quantitative imaging analysis of chest computed tomography (qCT) represents an alternative, and increasingly feasible, approach. We evaluated the role of qCT in RA-ILD by comparing to PFTs, respiratory patient-reported outcomes (PROs), and evaluating its prognostic value for survival.
Methods: We performed cross-sectional and cohort analyses using a multicenter, prospective cohort of patients with RA-ILD. Patients fulfilling ACR criteria for RA who were diagnosed with ILD by their treating clinician and had supporting imaging findings were enrolled between 1/2021 and 2/2025. qCT analysis was performed on baseline non-contrast chest CT as part of routine clinical care using the 3D SLICER Chest Imaging Platform. High attenuation areas between -600 and -250 Hounsfield units were quantified by the percentage of lung voxels in six lung regions to assess ILD (%HAA), with higher values indicating a greater degree of lung involvement. Additional assessments completed among participants included PFTs (FVC, diffusion capacity [DLCO]) and respiratory PROs (University of California San Diego Shortness of Breath Questionnaire [UCSD SOBQ] and Leicester Cough Questionnaire [LCQ]). Participants’ vital status was reported by site investigators. We assessed the correlations of chest CT %HAA with PFTs and respiratory PROs using Pearson correlations, as well as associations with survival using Cox regression adjusting for age and sex.
Results: We studied 113 participants with RA-ILD from 9 sites in this prospective cohort. The cohort had a mean (SD) age of 70.4 (8.0) years, was primarily male (78.8%), had frequent smoking history (69.9%), a mean RA duration of 20.5 (14.2) years, and a mean ILD duration of 6.7 (8.0) years. Mean (SD) FVC % predicted was 87.7 (22.1), and DLCO % predicted was 58.3 (19.9). Mean total lung %HAA was 6.2, with higher values in the lower lung regions (9.2 and 9.9) compared with the upper regions (4.3 and 3.5). qCT %HAA parameters were weakly to moderately negatively correlated with FVC (range r -0.22 to -0.37; p< 0.05) and DLCO (range r -0.22 to -0.35; p< 0.05) (Table 1). Lung %HAA was not associated with respiratory PROs. Over 169 patient-years of follow-up, 17 deaths occurred. Patients with higher %HAA tended to have poorer survival (range aHR 1.26 to 1.74 per 10 %HAA; Figure 1), though findings did not reach statistical significance. While FVC was similarly not significantly associated with survival, higher UCSD SOBQ scores, but not LCQ scores, were associated with poorer survival (per 10 units, aHR 1.22 [1.01, 1.48]).
Conclusion: In this study, qCT %HAA was weakly to moderately correlated with FVC and DLCO percent predicted in a multicenter, prospective RA-ILD cohort. Over an initial follow-up period with a limited number of deaths, qCT %HAA appeared to provide similar prognostic information on survival as FVC % predicted. These findings highlight a potential role for chest CT quantitative analysis to characterize and monitor RA-ILD.
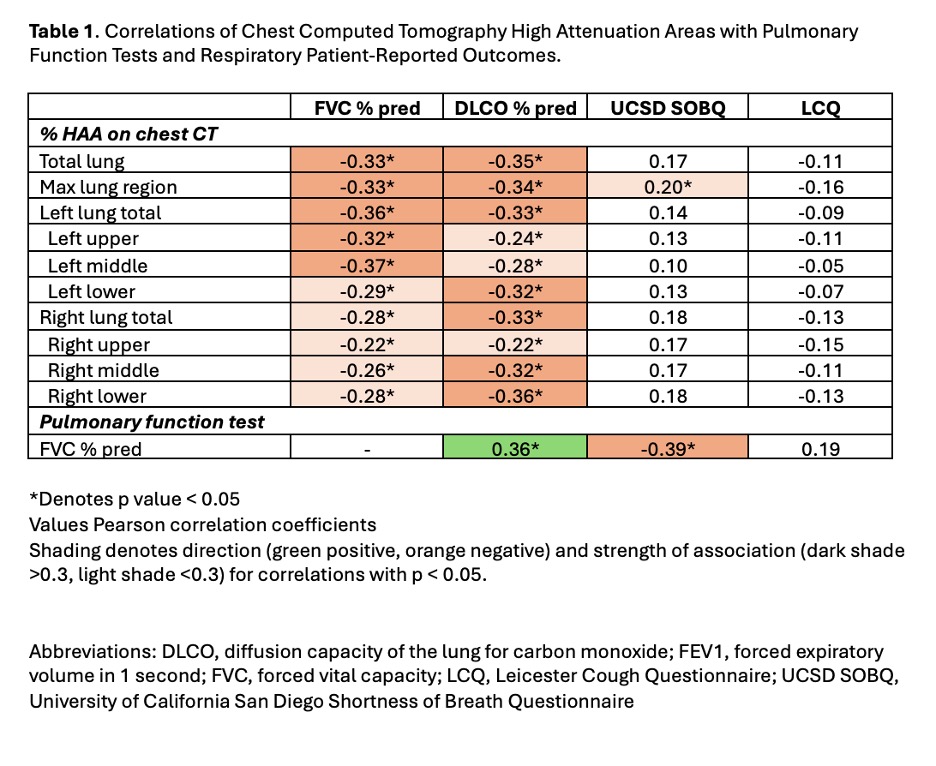 Table 1. Correlations of Chest Computed Tomography High Attenuation Areas with Pulmonary Function Tests and Respiratory Patient-Reported Outcomes.
Table 1. Correlations of Chest Computed Tomography High Attenuation Areas with Pulmonary Function Tests and Respiratory Patient-Reported Outcomes.
.jpg) Figure 1. Associations of Chest Computed Tomography High Attenuation Areas, Forced Vital Capacity, and Respiratory Patient-Reported Outcomes with Survival.
Figure 1. Associations of Chest Computed Tomography High Attenuation Areas, Forced Vital Capacity, and Respiratory Patient-Reported Outcomes with Survival.
To cite this abstract in AMA style:
Anthone E, Wan E, Schreiner A, Wysham K, Kunkel G, Cannon G, Reimold A, Richards J, Ascherman D, Kerr G, Monach P, Frideres H, Roul P, Matson S, Baker J, Mikuls T, England B. Quantitative Imaging Analysis of Chest Computed Tomography in Rheumatoid Arthritis-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/quantitative-imaging-analysis-of-chest-computed-tomography-in-rheumatoid-arthritis-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/quantitative-imaging-analysis-of-chest-computed-tomography-in-rheumatoid-arthritis-associated-interstitial-lung-disease/
