Session Information
Date: Sunday, November 13, 2022
Title: Vasculitis – ANCA-Associated Poster II: Treatment Efficacy, Clinical Outcomes, Biomarkers
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Although pulmonary manifestations occur frequently in AAV, empirical evidence of their impact on pulmonary function is scarce. This project analyzed PFT data from a large cohort of patients with granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA) to quantify a possible change in lung function. In addition, PFT results were tested for a correlation with findings on chest CT and X-ray.
Methods: Patients with diagnosed AAV according to ACR criteria and valid PFT were identified from the database of our vasculitis center in a tertiary university hospital. Cases with acute pulmonary comorbidities unrelated to AAV were excluded. The data comprised forced vital capacity (FVCex), Tiffeneau-Index (rFEV1), total airway resistance (RAWtot), total lung capacity (TLC), residual volume (RV), and transfer factor (TLCO). Mean values were compared to the defined standard value of the population (100% predicted) and in terms of pulmonary manifestation. Therefore, t-Test or Mann-Whitney-U-Test on a significance level of α = 5% was used. Furthermore, PFT data were compared to findings from CT scan, X-ray, and bronchoscopy using multiple linear regression.
Results: In total, 147 AAV-patients (GPA: n=81; MPA: n=37; EGPA: n=29) were included, of which 98 had a history of pulmonary involvement (GPA: nP=50; MPA: nP=20; EGPA: nP=28). The mean age at the time of PFT was 58.2 ± 24.1 (GPA), 73.2 ± 19.0 (MPA), and 55.8 ± 20.8 (EGPA). Patients had a median disease duration of 8.0 ± 66.0 months.
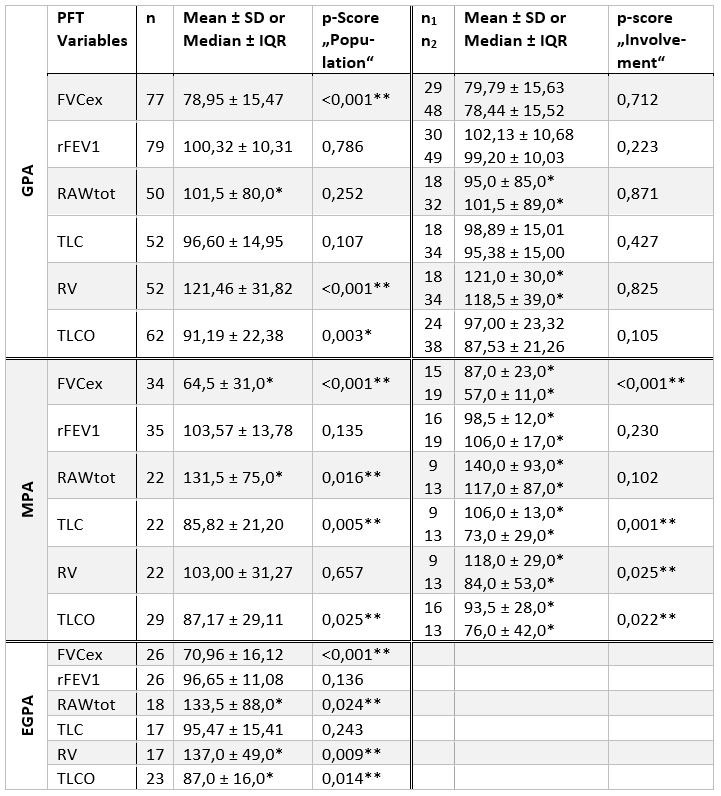
Table 1. For GPA, FVCex, RV and TLCO were statistically lowered compared to expected values of 100% predicted. However, there was no significant difference between patients with or without pulmonary manifestations. In patients with MPA, relevant impairments of FVCex, TLC and TLCO were observed compared to the standard population. These changes were significantly stronger in MPA-patients with pulmonary involvement. Statistically remarkable for EGPA-patients was an elevation of RAWtot and RV as well as a lowered TLCO.
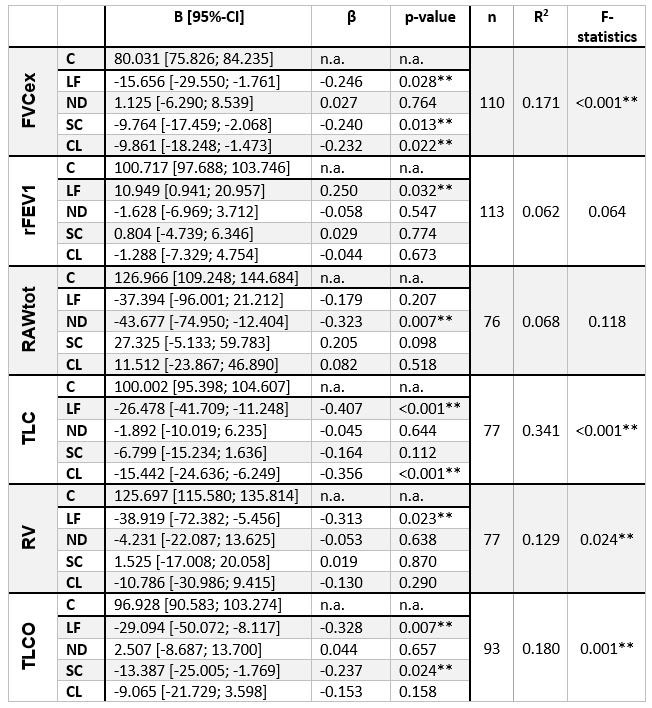
Table 2. All models except for rFEV1 and RAWtot were statistically significant. Lung fibrosis was correlated with an impairment of FVCex, TLC, RV, and TLCO between 16 to 39%. Patients with scarring showed lowered measures for FVCex plus TLCO, and consolidations were connected to a reduction of FVCex as well as TLC. There was no statistically significant correlation provable between PFT and emphysema, bronchial involvement, stenosis, or diffuse alveolar hemorrhage.
Conclusion: MPA shows a restrictive ventilatory defect and a lowered diffusion capacity that is both attributable to the AAV and more common in patients with pulmonary fibrosis. As expected, many patients with eGPA have an obstructive ventilatory pattern. AAV-patients with scarring seem to suffer more often from impaired diffusion capacity whereas patients who show signs of consolidation do have a higher risk for a restrictive pattern. The interpretation of our data is limited by the potential indication bias for PFT and the retrospective design. Summing up, PFT should be included in future prospective clinical trials in patients with AAV.
PFT values are expressed as percentage of predicted. On the left: comparison with 100% predicted of population. On the right: comparison between patients without (n1, first row) and with (n2, second row) pulmonary manifestation. Depending on the presence of Gaussian distribution bidirectional unpaired t-test or Mann-Whitney-U-test with a significance level of α = 5% were used for statistical analysis. Regarding to this mean value or median (*) was quoted. Significant p-values are marked with (**).
PFT values are expressed as percentage of predicted. Constant (C), diagnosed lung fibrosis (LF), nodules (ND), scarring (SC), consolidation (CL). Not displayed: emphysema, bronchial involvement, stenosis, and diffuse alveolar hemorrhage. Statistical method: Multiple linear regression. B = regression coefficient (95%-CI), β = standardized coefficient, n = number of standardized residuals, R2 = adapted correlation coefficient, F-statistics = describes the significance of the model, significant results are marked with (**).
To cite this abstract in AMA style:
Dieterich J, Feng Y, Mahrhold J, El Rai A, Hellmich B. Pulmonary Function Testing (PFT) in Patients with Antineutrophil Cytoplasmic Antibodies (ANCA)-associated Vasculitis (AAV): Correlation with Radiologic Imaging [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/pulmonary-function-testing-pft-in-patients-with-antineutrophil-cytoplasmic-antibodies-anca-associated-vasculitis-aav-correlation-with-radiologic-imaging/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pulmonary-function-testing-pft-in-patients-with-antineutrophil-cytoplasmic-antibodies-anca-associated-vasculitis-aav-correlation-with-radiologic-imaging/