Session Information
Date: Sunday, November 7, 2021
Title: Measures & Measurement of Healthcare Quality Poster (0623–0659)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: The COVID-19 pandemic forced the provision of telehealth care to rheumatology patients with a broader range of diagnoses and disease activity than previously studied. In this study we seek to understand factors that associate with providers’ perceptions of telehealth utility.
Methods: From 10/1/2020 – 1/31/2021, six providers at an academic medical center rated their telehealth visits according to perceived utility in making treatment decisions using the following Telehealth Utility Score (TUS) (1 = very low to 5 = very high). Ratings were entered immediately following each visit. ‘Low telehealth utility’ visits had a TUS between 1- 3 and ‘high telehealth utility’ visits had a TUS between 4-5. Providers also documented a provider global assessment of disease activity (0 = no activity to 10 = high activity). Data were obtained through the electronic data warehouse and manual chart review. Modified poisson regression models with robust error variance were used to assess the association between low versus high TUS and encounter diagnoses, current and prior patient-reported disease activity (RAPID3), provider global, and medication changes during the visit. Each analysis was performed unadjusted and adjusted according to age, race, insurance, and encounter mode (video/phone).
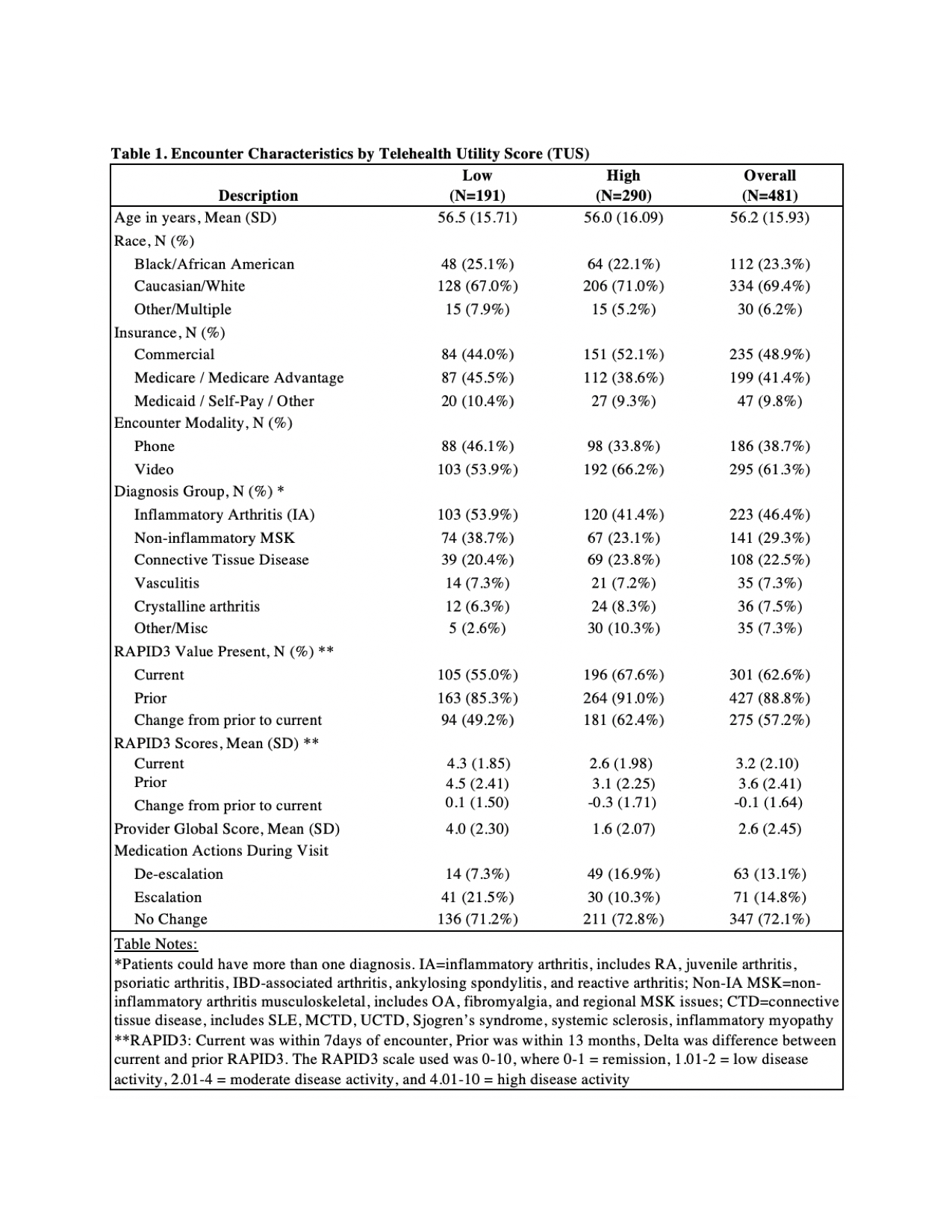
Results: A total of 481 telehealth encounters were included, of which 191 (39.7%) had a low telehealth utility score (Table 1). Patients with a diagnosis of inflammatory arthritis (IA) were more likely to have low telehealth utility compared to those with other diagnoses in unadjusted and adjusted models (aRR 0.806, 95% CI: 0.695-0.934, p=0.004). Furthermore, in patients with IA, the addition of a non-inflammatory musculoskeletal diagnosis made a telehealth encounter more likely to be of low utility in unadjusted and adjusted models (aRR 0.537, 95% CI: 0.344-0.838, p=0.006).
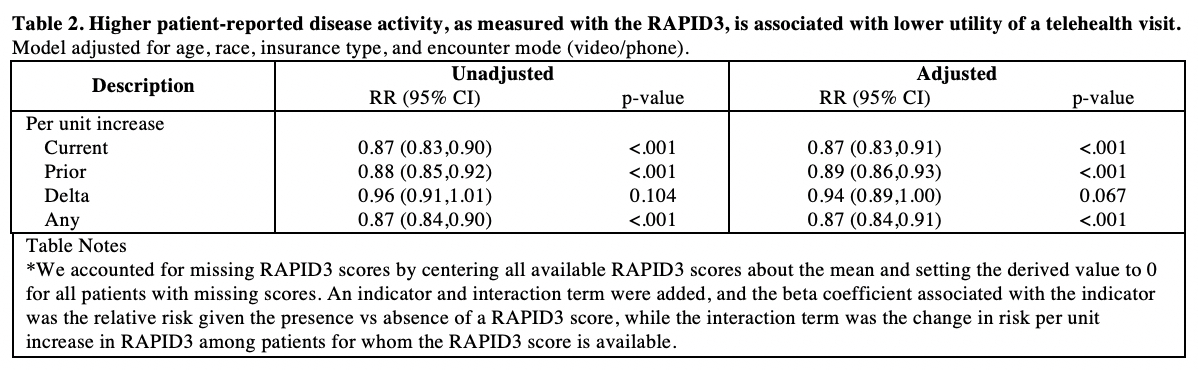
Higher patient and provider-reported measures of disease activity were significantly associated with low telehealth utility in unadjusted and adjusted models (Table 2), as follows: current RAPID3 (aRR 0.87, CI: p< 0.001), prior RAPID3 (aRR 0.89, p< 0.001), and provider global (aRR 0.83, 95% CI 0.79-0.87, p< 0.001).
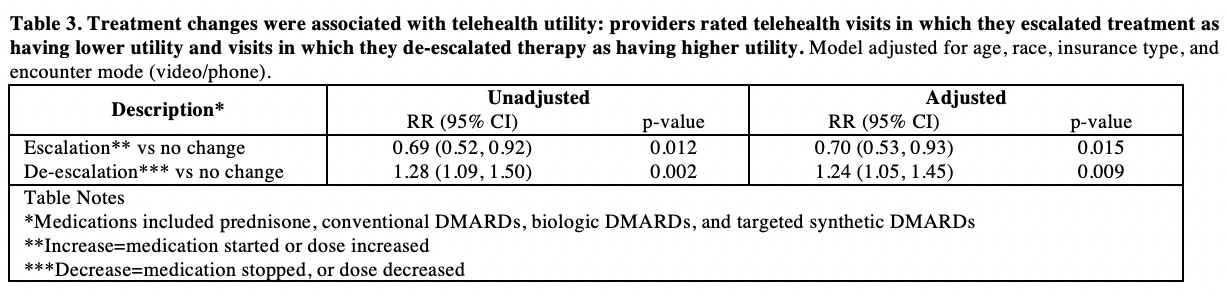
An escalation in rheumatologic treatment was associated with low telehealth utility (aRR 0.7, p=0.015) and a de-escalation in rheumatologic treatment was associated with high telehealth utility (aRR 1.24, p=0.009), see Table 3.
Conclusion: Overall, telehealth was rated as a useful mode of care delivery for the majority of visits. A diagnosis of IA was associated with low telehealth utility, especially if a non-IA musculoskeletal diagnosis was also present, highlighting the need for in-person care for patients with active musculoskeletal symptoms. Intriguingly, higher disease activity by current and prior RAPID3 was associated with lower telehealth utility, suggesting that disease activity measures could help determine appropriateness for telehealth care. Finally, medication changes were associated with TUS, suggesting that providers feel comfortable decreasing medications during telehealth visits but prefer to escalate therapy in-person.
To cite this abstract in AMA style:
Howe C, Smith I, Overton R, Henao R, Economou-Zavlanos N, Doss J, Clowse M, Leverenz D. Provider Assessment of Telehealth Utility During COVID-19 [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/provider-assessment-of-telehealth-utility-during-covid-19/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/provider-assessment-of-telehealth-utility-during-covid-19/