Session Information
Date: Sunday, November 8, 2020
Title: Epidemiology & Public Health Poster III: Inflammatory Rheumatic Disease
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatoid arthritis (RA) may have up to a 15% increased risk of prostate cancer per a recent meta-analysis (Simon et al. Arthritis Research & Therapy, 2015). Previously, we found similar rates of prostate cancer in U.S. Veterans with RA as in individuals from the general population via indirect standardization using the Surveillance, Epidemiology, and End Results (SEER) Program (Brittan et al, Abstract #943, 2018). Recognizing the potential for bias based on the referent population and differences in cancer surveillance, we compared the risk of prostate cancer among RA and non-RA patients in the Veterans Health Administration (VHA; direct standardization).
Methods: We performed a retrospective, matched cohort study in the VHA from 2000 to 2018. We identified male patients with RA using a validated administrative algorithm and matched them to male patients without RA (no RA diagnostic codes or DMARDs) on age and enrollment year (up to 1:5). RA and non-RA patients with prior prostate cancer or prostatectomy were excluded. Prostate cancer and prostate cancer death were identified from the VA oncology domain within the Corporate Data Warehouse and the National Death Index. Multivariable Cox models compared prostate cancer risk after adjusting for race, smoking status, body mass index, Agent Orange exposure, Rheumatic Disease Comorbidity Index score, prostate-specific antigen testing, and health care utilization. Subjects were clustered by the matched RA/non-RA groups. Recognizing the potential for greater retention in the healthcare system and premature mortality among RA patients to influence results, we tested additional models censoring for a gap of >365 days between VA visits and censoring the matched patients at the time of death (in cases unrelated to prostate cancer) in RA patients.
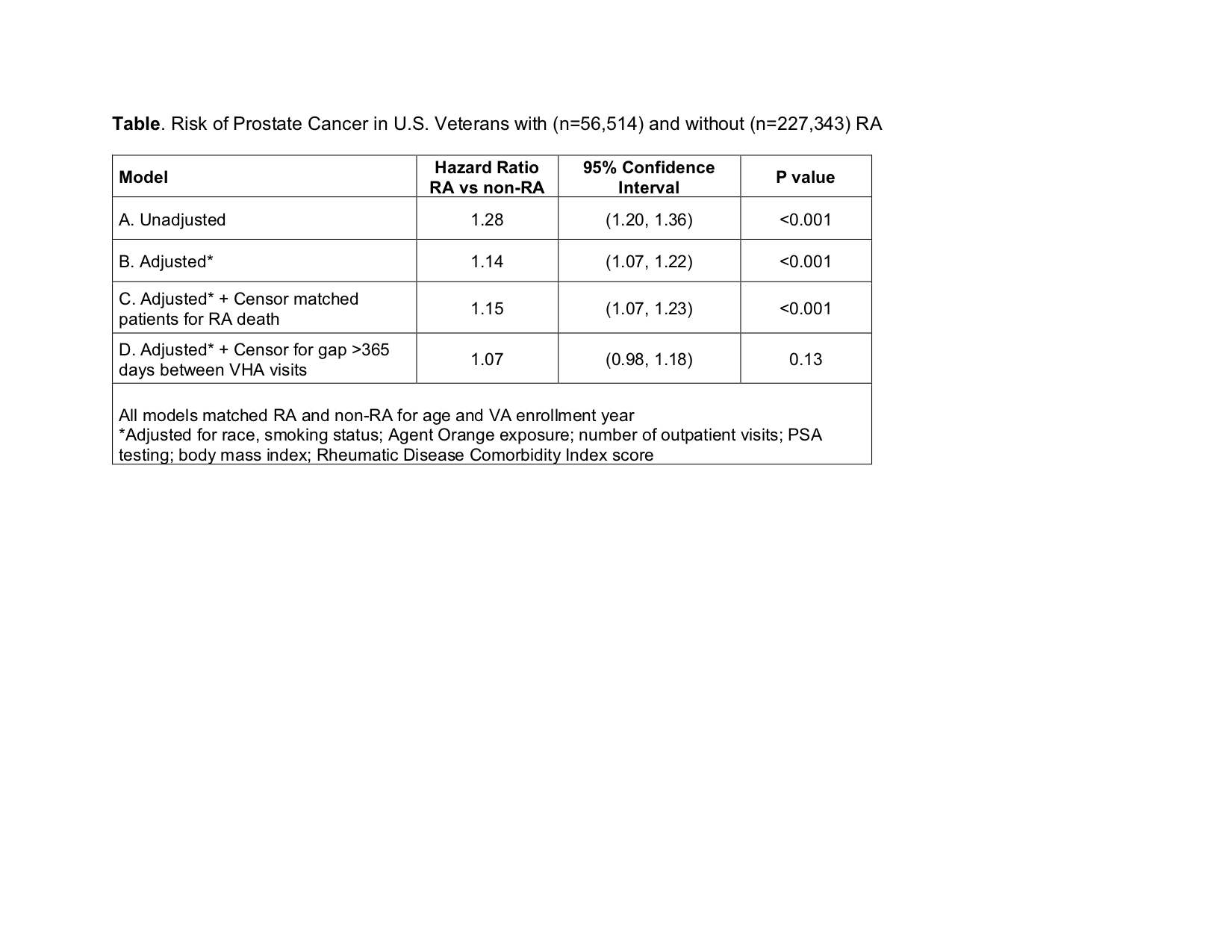
Results: We included 56,514 Veterans with RA and 227,343 Veterans without RA. Mean (SD) age was 64 (11) years and the majority (74% RA, 88% non-RA) were Caucasian. There were 6,550 incident prostate cancers during 2,337,104 patient-years of follow-up. Prostate cancer incidence rates (per 1,000 patient-years) were 3.5 (95% CI 3.3-3.7) in RA and 2.7 (95% CI 2.6-2.7) in non-RA. There was a 28% increased risk of prostate cancer in RA (Model A; Table) that was attenuated to 15% after multivariable adjustment (Model B). Accounting for premature mortality in RA from other causes did not meaningfully affect results (Model C). However, after censoring for a gap of >365 days between VA visits, RA was not significantly associated with prostate cancer risk (Model D: HR 1.07; 95% CI 0.98-1.18; p=0.13). Several sensitivity analyses produced results consistent with the primary results.
Conclusion: Using direct standardization and accounting for relevant confounders and causes of potential bias, we did not find RA to be associated with an increased risk of prostate cancer. These findings highlight the importance of accounting for healthcare system retention when studying cancer risk in rheumatic diseases to prevent detection bias.
To cite this abstract in AMA style:
Brittan K, Roul P, Baker J, Yang Y, Sauer B, Singh N, Sayles H, Cannon G, Mikuls T, England B. Prostate Cancer Risk Is Not Increased in Rheumatoid Arthritis After Accounting for Retention in a Health Care System [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/prostate-cancer-risk-is-not-increased-in-rheumatoid-arthritis-after-accounting-for-retention-in-a-health-care-system/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prostate-cancer-risk-is-not-increased-in-rheumatoid-arthritis-after-accounting-for-retention-in-a-health-care-system/