Session Information
Date: Sunday, November 17, 2024
Title: Metabolic & Crystal Arthropathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Carotid atherosclerosis is prevalent in patients with gout. A prior cross-sectional study at our hospital demonstrated an association between tophi and positive Power Doppler (PD) signal with atheroma plaques.
This study aims to explore the association between the evolution of carotid atherosclerosis with changes in echographic deposit signs and inflammation.
Methods: The prospective cohort study included 103 patients with new crystal-proven gout, 94% men, with a mean baseline age of 62 years, and 17% with tophaceous gout.
Three ultrasound assessments were performed: baseline (M0), at six months (M6), and at 12 months (M12). The same trained sonographer, blinded to clinical data, performed these repeated assessments.
M0 included A) scan of bilateral carotid to evaluate intima-media thickness (IMT) and atheroma plaques, according to Mannheim consensus, and B) musculoskeletal (MSK) scans in wrists, second metacarpophalangeal (2MCPs) and first metatarsophalangeal (1MTPs) joints, and tricipital and patellar tendons, evaluating urate crystal deposit signs (double contour, hyperechoic aggregates, and tophi, according to OMERACT definitions) and local PD signal.
M0 was performed without urate-lowering therapy, but prophylactic agents were allowed. Subsequently, patients were treated in parallel in clinical practice.
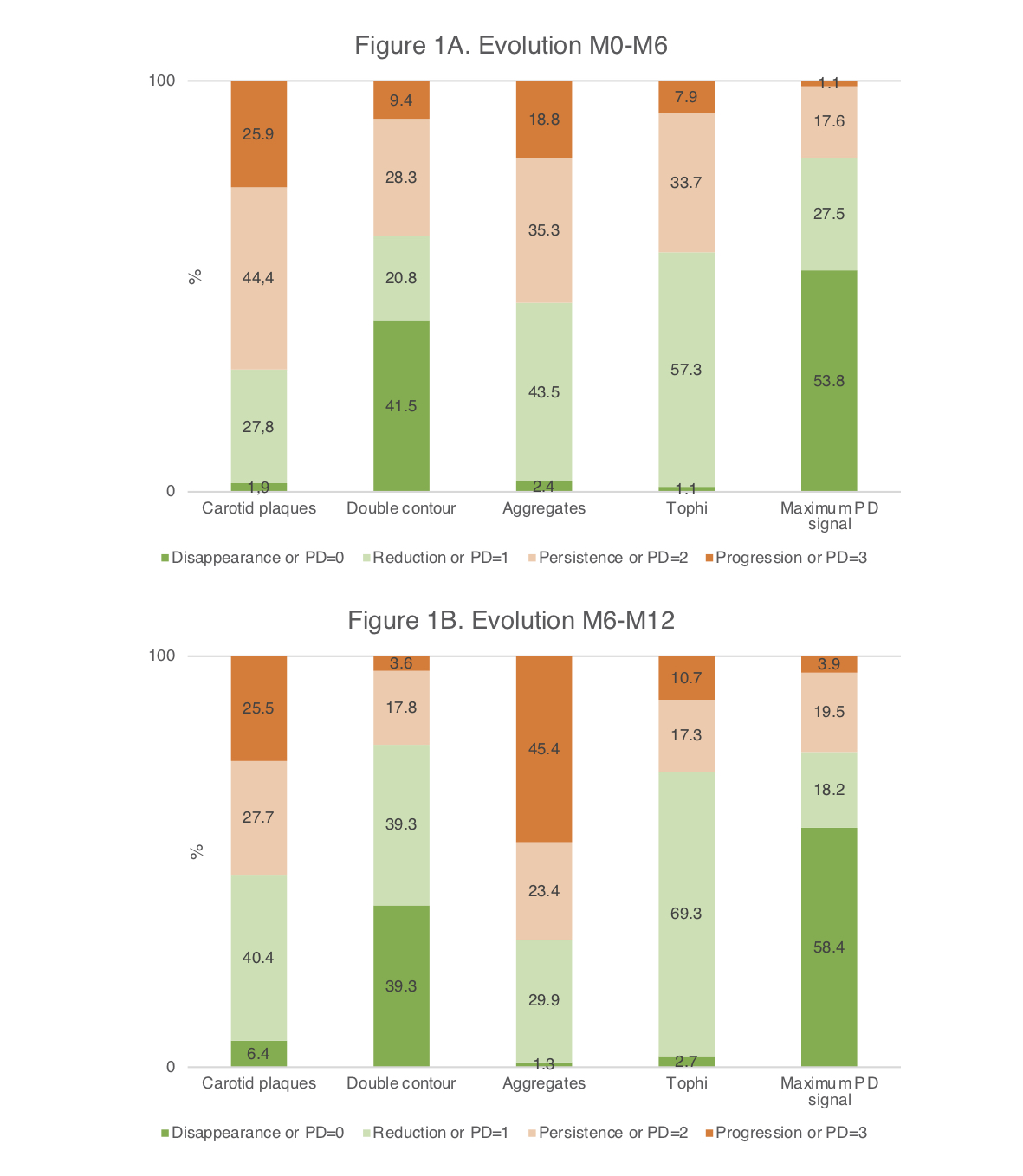
At M6 and M12, carotid and MSK ultrasound evaluation at locations with baseline deposits (M0) was repeated. The sonographer classified the evolution of deposits and carotid plaques as “disappearance,” “reduction,” “persistence,” and “progression”. We later dichotomized plaque and deposit variables into “disappearance/reduction” or “persistence/progression” for statistical analyses. The maximum value in all evaluated locations was taken for the PD signal. The association between changes in carotids, deposits, and maximal PD signal was studied using the Chi-square test and Fisher’s exact test.
Results: Of 103 patients, 91 (88.3%) and 78 (75.7%) underwent M6 and M12 evaluations, respectively. At M0, the mean number of locations with deposits and a positive PD signal was 9.9 (SD 4.1) and 1.1 (SD 1.1). Fifty-nine percent had carotid atheroma plaques; the mean IMT was 0.82 mm (SD 0.21).
Figure 1 shows the evolution of carotid plaques, urate deposits, and PD signal. IMT persisted unchanged at M6 and M12. At M6, no association was found between carotid and MSK variables. At M12, the reduction or disappearance of atheroma plaque was significantly associated with the absence of a PD signal, compared to a persistent PD signal (64.0% vs. 28.6%, p=0.017). Improvement in carotid plaques was unrelated to improvements in double contour signs (62.5% vs. 0%, p=0.087), aggregates (57.9% vs. 37%, p=0.162), and tophi (48.4% vs. 42.9%, p=0.731). High-intensity statins was also associated with the reduction or disappearance of atheroma plaques. No relationship was found with other clinical or analytical variables.
Conclusion: After 12 months of urate-lowering treatment in gout patients, improvements in carotid atheroma plaques were more common in those with an absent PD signal. This adds evidence to the link between crystal-driven inflammation and atherosclerosis in patients with gout.
To cite this abstract in AMA style:
Rodríguez Alvear C, Martínez Sanchís A, Calabuig Sais I, Andrés M. Prospective Evaluation of Carotid Atherosclerosis, Urate Deposits and Inflammation After One Year of Treatment in Newly Diagnosed Gout [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prospective-evaluation-of-carotid-atherosclerosis-urate-deposits-and-inflammation-after-one-year-of-treatment-in-newly-diagnosed-gout/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prospective-evaluation-of-carotid-atherosclerosis-urate-deposits-and-inflammation-after-one-year-of-treatment-in-newly-diagnosed-gout/