Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Pneumocystis jirovecii Pneumonia (PJP) is an opportunistic infection that may affect immunocompromised patients. PJP prophylaxis has been recommended for some autoimmune diseases but not others. The purpose of this study was to use the electronic health records from the national Veterans Affairs database to examine the incidence of PJP and PJP prophylaxis-related adverse events among patients with ANCA associated vasculitis (AAV), systemic lupus erythematosus (SLE), immune-mediated inflammatory myopathies (IIM), and giant cell arteritis (GCA).
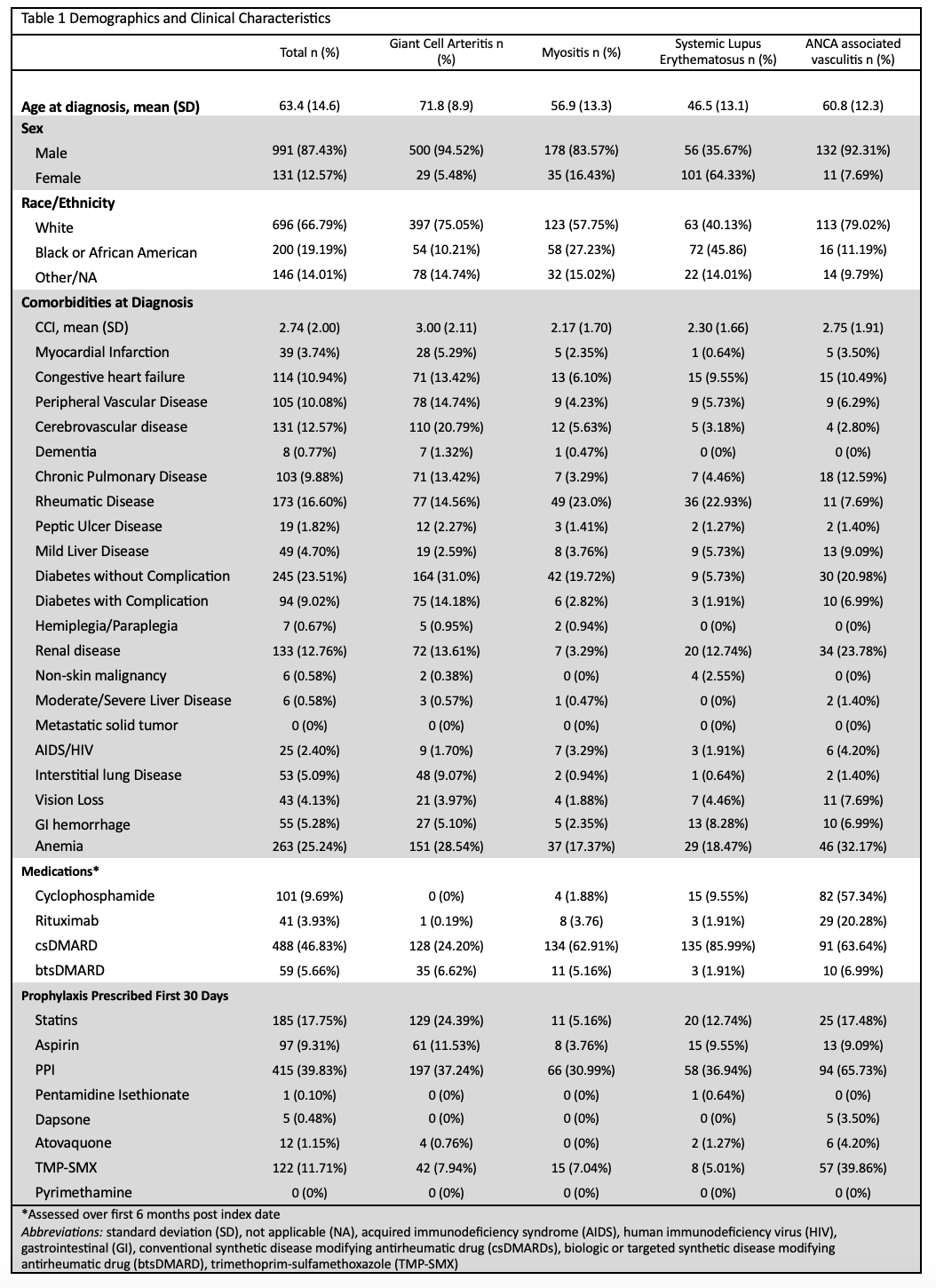
Methods: We performed a retrospective cohort analysis utilizing the VA database. Patients were required to have a diagnosis code for SLE (ICD-9-CM 710.0, ICD-10-CM M31.1x), AAV (ICD-9-CM 446.[04], ICD-10-CM M30.[01], M31.3[01], M31.7), GCA (ICD-9-CM 446.5, ICD-10-CM M31.[56]), or myositis (ICD-9-CM 359.71, ICD-10CM M33.[129], M60.[89]x) as well as the following: ≥ 2 inpatient or outpatient encounters, ≥ 2 rheumatology visits during the study period, and ≥20mg/day of prednisone for at least 30 days within 30 days following their first rheumatology encounter, which was defined as the index date. Patients were stratified by disease and whether they received PJP prophylaxis, which was defined by any prescription for an antibiotic to treat PJP within 30 days of the index date. PJP infection was defined by any diagnostic code for PJP and was assessed over the first 6 and 12 months of therapy. PJP prophylaxis related adverse events were also collected and included the following: adverse drug reaction (ICD9 995.0, 995.20, ICD10 T50.905A), rash (ICD9 781.1, ICD10 R21.x), methemoglobinemia (ICD9 289.7, ICD10 D74.9), nephropathy (ICD9 58[0346].x, ICD10 N17.x), hemolytic anemia (ICD9 283.9, ICD10 D59.9), or neutropenia (ICD9 288.0[39], ICD10 D70.[89]). Adjusted odds ratios (OR) for adverse events commonly associated with PJP prophylaxis were estimated using stepwise logistic regression.
Results: A total of 1042 patients were identified with a mean age of 63.4 years, the majority whom had GCA (50.77% and were male (87.43%) and white (66.79%). The most common PJP prophylaxis was trimethoprim/sulfamethoxazole (12.67%). Eight patients were diagnosed with PJP by diagnostic codes (6 month incidence 15.73 per 1000 patient years (py), 12 month incidence 7.78 per 1000 py), including 3 with AAV (6 month incidence 44.31 per 1,000 py, 12 month incidence 21.87 per 1,000 py), 4 with GCA (6 month incidence 15.45 per 1,000 person years, 12 month incidence 7.66 per 1,000 py), and one with myositis (6 month incidence 9.55 per 1,000 py, 12 month incidence 4.73 per 1,000 py). After adjusting for sex, race, CCI, and medications prescribed prior to induction therapy, the odds of experiencing an adverse event were three-fold higher among those who received prophylaxis (OR 3.1, 95% CI 1.81-5.35).
Conclusion: In a large study of patients in the VA database with AAV, GCA, IIM, or SLE, the incidence of PJP was low. Patients with AAV had the highest incidence of PJP and prophylaxis was associated with adverse events. Additional analysis using laboratory data and direct review of patient charts will be conducted.
To cite this abstract in AMA style:
Lungova K, Sherman K, Mirza M, Mehta R, Putman M. Prophylaxis Against Pneumocystis Jerovecii Pneumonia for Patients with Systemic Autoimmune Diseases: Analysis of the Veterans Affairs Database [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prophylaxis-against-pneumocystis-jerovecii-pneumonia-for-patients-with-systemic-autoimmune-diseases-analysis-of-the-veterans-affairs-database/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prophylaxis-against-pneumocystis-jerovecii-pneumonia-for-patients-with-systemic-autoimmune-diseases-analysis-of-the-veterans-affairs-database/