Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: SLE-related outcomes are traditionally assessed by clinician-derived measures. However, these assessments often do not fully capture how patients experience their disease. We assessed the alignment between patient-reported outcomes measurement information system (PROMIS) and disease activity measures in patients with SLE.
Methods: This cross-sectional study, based on the Lupus Cohort at Beth Israel Deaconess Medical Center, spanned from October 2023 to April 2024. Participants were diagnosed with SLE according to the 2019 ACR/EULAR criteria. CRP, SLEDAI, and Physician Global Assessment (PGA) were recorded at each visit. Patients completed the PROMIS-29 v2.1 questionnaire using the REDcap® database, covering domains such as physical function, fatigue, pain interference, depression, anxiety, social participation, and sleep disturbance. T-scores for the seven PROMIS domains and the pain impact score were calculated using the “Health Measures” PROMIS Assessment Center tool. We used Spearman rank correlations to explore relationships between PROMIS T-scores and clinical assessments. Linear and logistic mixed-effects models were used for continuous and binary variables. Patients were stratified into low-activity (SLEDAI ≤ 4; PGA ≤ 1) and high-activity (SLEDAI > 4; PGA > 1) groups.
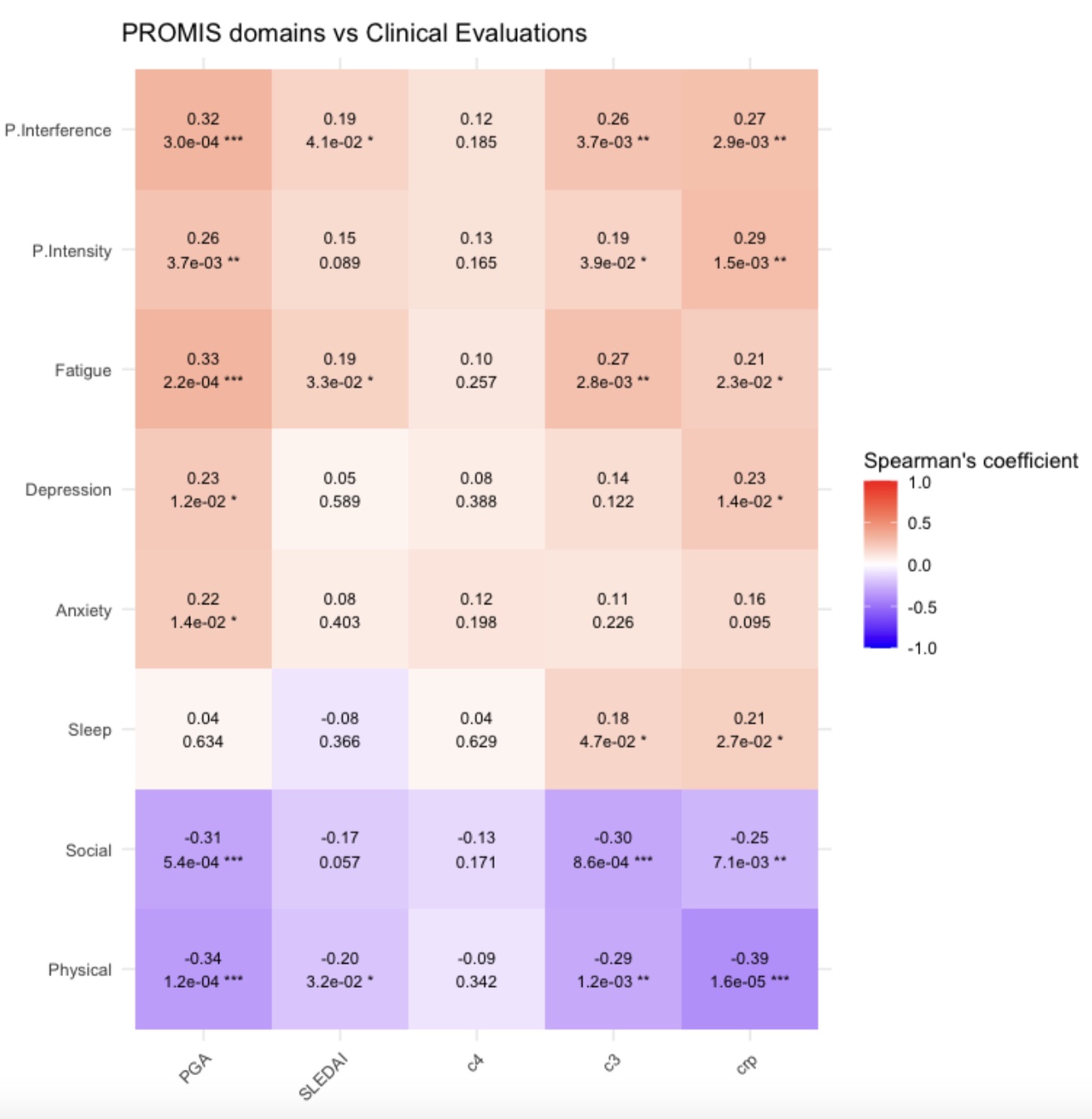
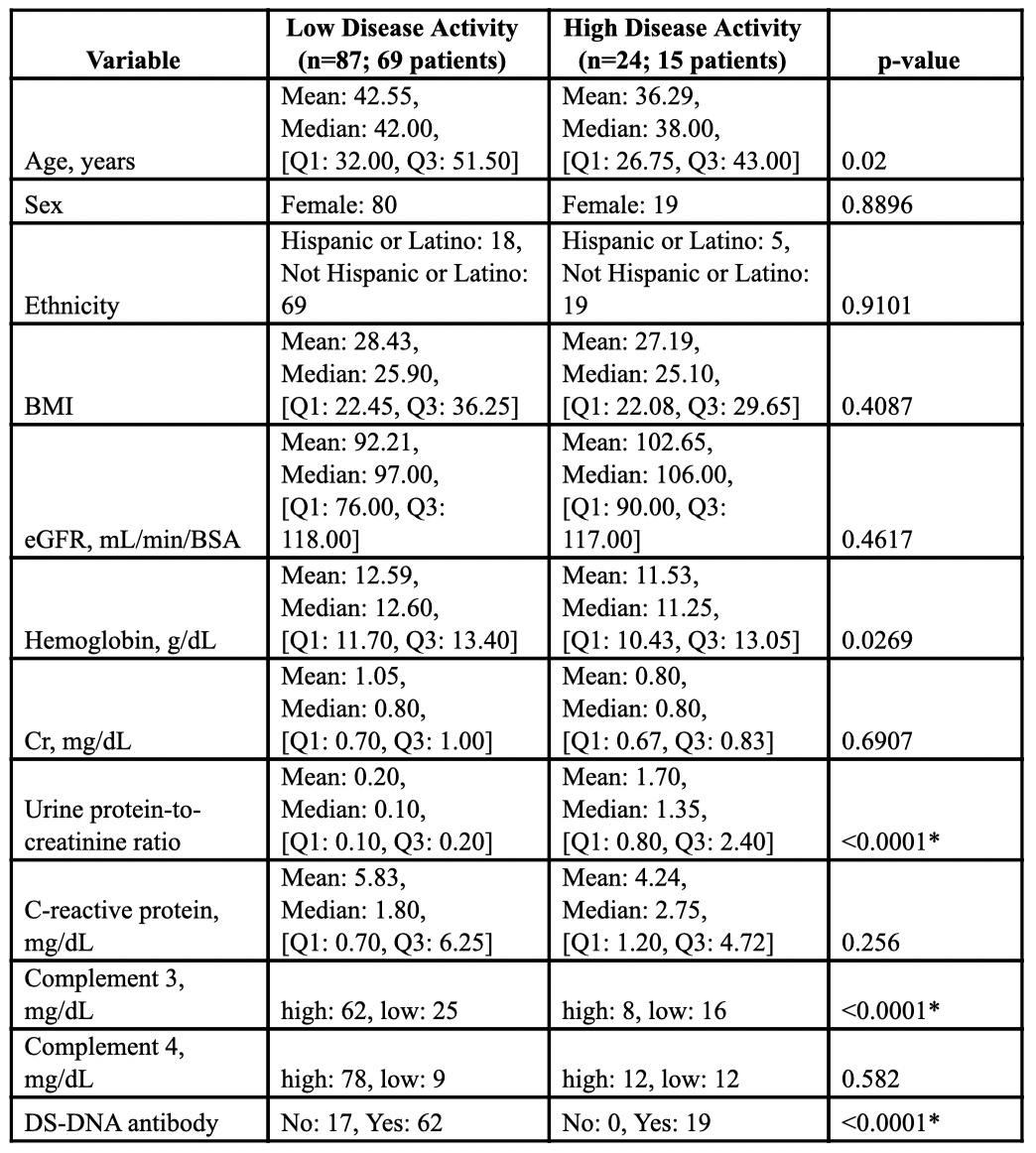
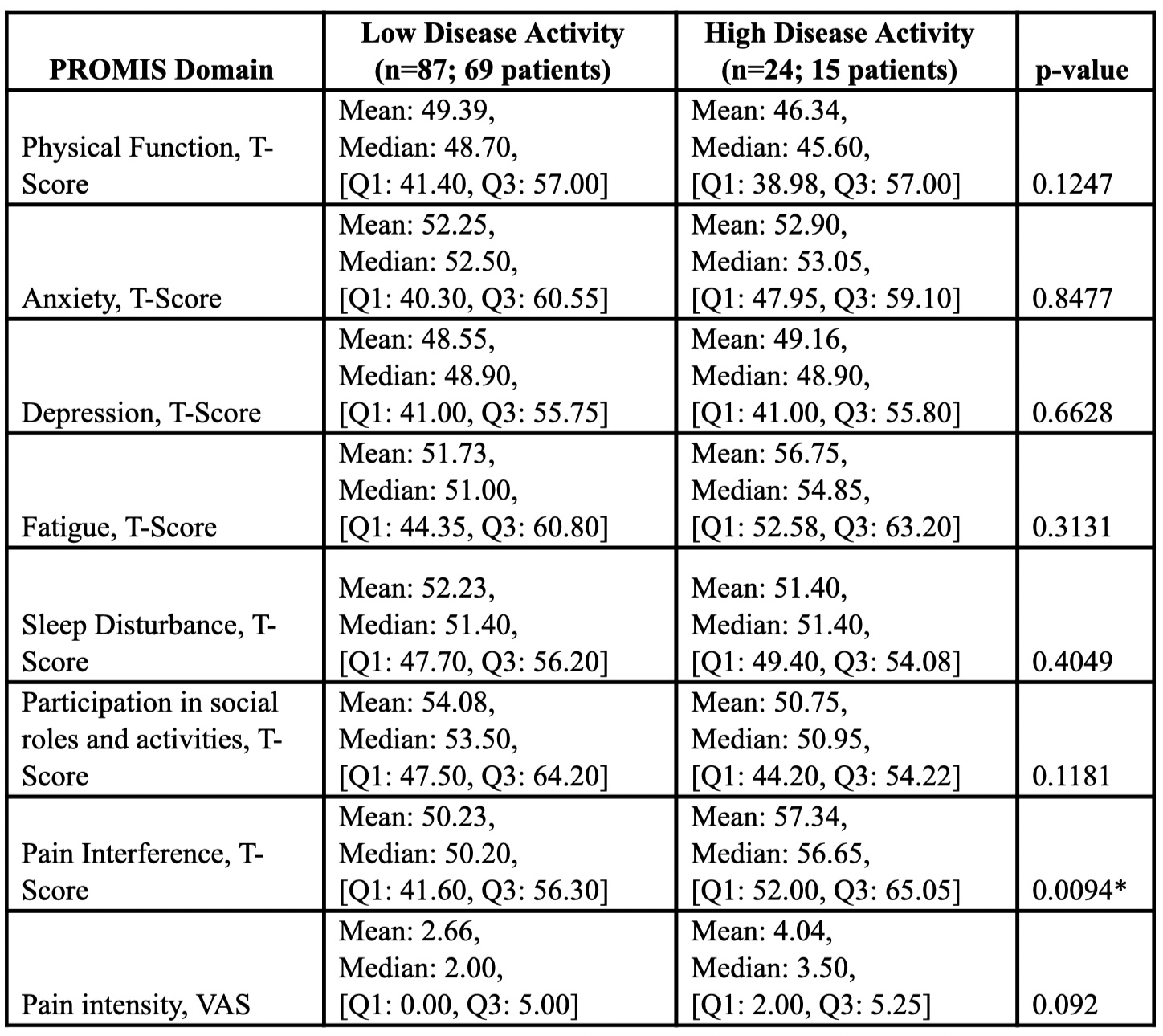
Results: 92 patients, predominantly female (83.6%), with an average age of 43.6 years and a mean BMI of 28 (Table 1) were included in this study. Initial assessments showed a mean SLEDAI of 4.19 (±3.42) and a median PGA score of 0.5. Correlation analysis (Figure 1) showed that increased disease activity and inflammation negatively affected Physical Function and Social Participation, as these domains inversely correlated with PGA, SLEDAI, and CRP. Conversely, the Fatigue, Pain Interference, and Pain Intensity domains showed positive correlations with PGA, SLEDAI, indicating that as disease activity measures increase, so do symptoms that impact quality of life. Significant differences in the Pain Interference domain were observed when patients were divided into low and high disease activity groups (Table 2).
Conclusion: Our study highlights significant correlations between increased SLE activity and deterioration in patient-reported outcomes. CRP’s correlation with Pain Intensity and Interference, Fatigue, Sleep Disturbance, and Depression is noteworthy, as this biomarker is usually not a direct indicator of SLE activity, except in specific conditions like arthritis and serositis. These findings suggest that CRP may play a broader role in some SLE cases, pointing to the need to reevaluate SLE monitoring and management, especially regarding pain and psychosocial aspects. Integrating both PROMIS surveys and CRP measurements with clinical assessments can guide treatment decisions to improve outcomes in SLE patients. Future analyses will explore the impact of therapy adjustments on PROMIS scores and provider assessments of SLE activity.
To cite this abstract in AMA style:
Korogodina A, Sundel E, Markov Y, Kyttaris V, O'Connell J, Krishfield S. PROMISing Outcomes: Understanding the Concordance Between Provider-assessment and Patient-reported Disease Activity in SLE [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/promising-outcomes-understanding-the-concordance-between-provider-assessment-and-patient-reported-disease-activity-in-sle/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/promising-outcomes-understanding-the-concordance-between-provider-assessment-and-patient-reported-disease-activity-in-sle/