Session Information
Date: Friday, November 6, 2020
Title: Epidemiology & Public Health Poster I: COVID-19 & Rheumatic Disease
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Little is known about the general health and wellbeing of patients with systemic rheumatic diseases (SRD) during the COVID pandemic. We sought to compare health related quality of life in patients with and without SRD during the height of the COVID-19 pandemic in New York City.
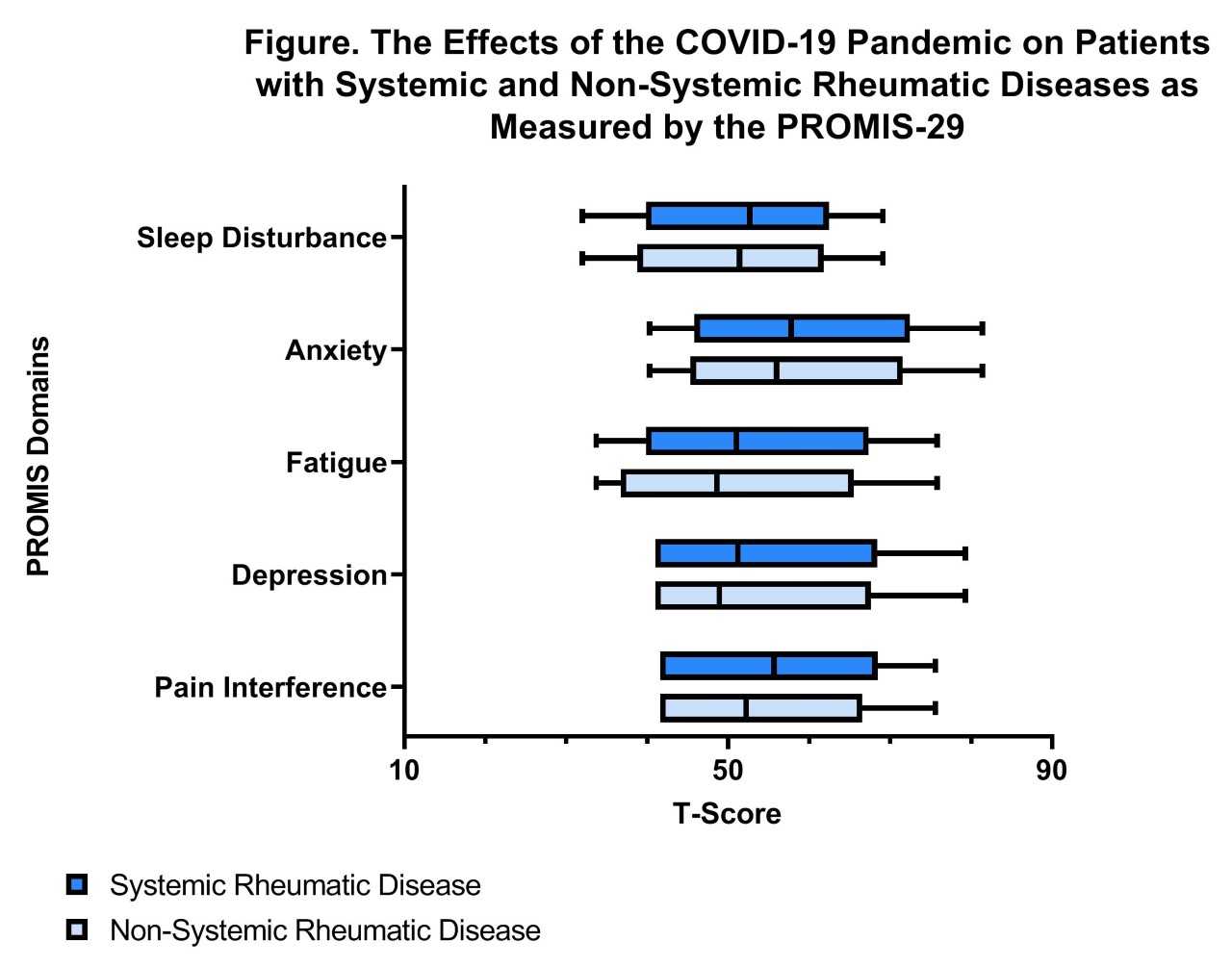
Methods: We emailed a secure web-based survey to 26,045 patients aged ≥18 years who were evaluated at least once by a rheumatologist during the two years prior to April 1, 2020 at a tertiary care academic center in New York City. Patients were invited to complete the survey by email or phone between April 24, 2020 and May 26, 2020. Information collected included self-reported COVID-19 diagnosis, potential COIVD-19 symptoms, rheumatic disease diagnosis, and sociodemographic factors. Respondents completed 5 domains from the PROMIS-29 (depression, anxiety, sleep disturbance, fatigue, pain interference). PROMIS-29 results were transformed to T-scores, with 50 being the mean for the US population, and a difference of 5 points considered to be clinically meaningful. Wilcoxon rank-sum, Fischer’s exact or chi-square tests were used, as appropriate, to compare demographics and PROMIS-29 scores in patients who reported having an SRD vs. those who did not.
Results: 6,584/26,045 (25.3%) respondents completed the PROMIS-29, and 4,147/6584 (62.9%) self-reported having an SRD. Most common SRDs included RA (N=1081, 26%), Psoriatic Arthritis/Spondyloarthritis (N=521,12.6%) and SLE (N=310, 7.5%). Patients with SRD were younger, less likely to be white and more likely to be Hispanic/Latino. Patients self-reporting an SRD were statistically significantly more likely to have had a confirmed close contact with a person with COVID-19 (22% vs. 20%; p=0.04), and spend > 95% of their time homebound (74% vs. 70%; p=0.0008). Those SRD patients who reported COVID-19 symptoms were more likely to exhibit their COVID-19 like symptoms for > 4 days compared to those without an SRD (42% vs. 37%; P< 0.0001) (Table 1). Across the five measured PROMIS-29 domains, patients with an SRD had worse scores than the population mean, and statistically significantly worse scores compared to those without SRD; however these differences were not clinically meaningful (Table 2 and Figure 1).
Conclusion: During the COVID-19 pandemic, patients with SRDs reported statistically significantly worse pain interference, depression, fatigue, and anxiety than the mean of the US population and those without SRD; however, these differences were not clinically meaningful. Patients with SRD were more likely to have had a confirmed close contact with someone with COVID-19, COVID-19 like symptoms for > 4 days, and were more likely to spend >95% of their time homebound compared to those without SRD. These data suggest that while patients with and without SRD had similar mental and physical health domains during the pandemic, SRD patients’ quality of life may be differentially impacted by COVID-19, due to longer disease course, increased social exposure to COVID-19 cases, and greater social isolation. Further study is needed to evaluate whether COVID-19 continues to differentially impact the life of patients with SRD as the pandemic progresses.
To cite this abstract in AMA style:
Vitone G, Frey M, Feldman C, Lally L, Bass A, Salmon J, Crow M, Lockshin M, Bykerk V, Barbhaiya M, Mandl L. PROMIS-29 and Health Related Quality of Life in Rheumatology Outpatients During the COVID-19 Pandemic in New York City [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/promis-29-and-health-related-quality-of-life-in-rheumatology-outpatients-during-the-covid-19-pandemic-in-new-york-city/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/promis-29-and-health-related-quality-of-life-in-rheumatology-outpatients-during-the-covid-19-pandemic-in-new-york-city/