Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Glucocorticoids (GCs) remain a cornerstone of treatment of ANCA-associated vasculitis (AAV) but predispose people to infectious, metabolic, and other toxicities. We projected the long-term clinical outcomes associated with different GC treatment strategies for AAV using AAV-Sim, a previously validated microsimulation model.
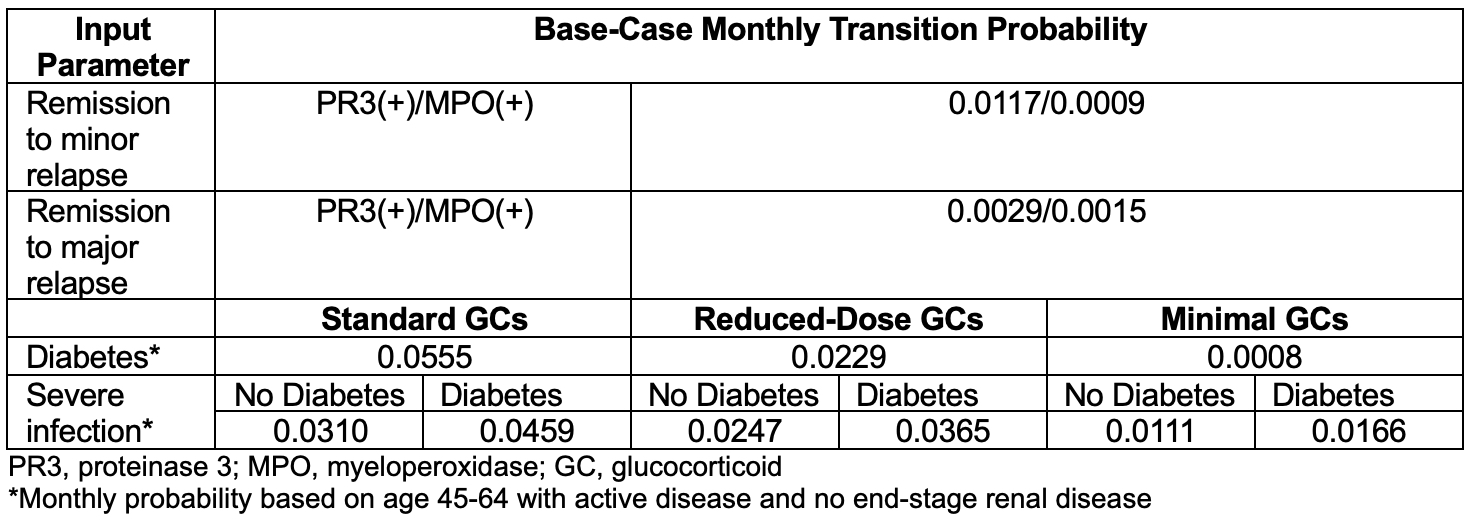
Methods: At model start, all individuals are in remission without diabetes. Each month, individuals in the model can transition between active (e.g., major/minor relapse) or inactive AAV states and are at risk of complications and death. Demographics, disease-specific characteristics, and monthly transition probabilities (Table 1) are derived from relevant literature (e.g., clinical trials in AAV, national mortality data, local AAV cohort) and stratified by demographic, disease-specific (e.g., sex, ANCA type), and treatment characteristics. The GC regimen affects risk of incident diabetes and severe infection; diabetes also directly increases the risk of severe infection, end-stage renal disease, and mortality. In combination with fixed-dose rituximab (every 6 months), we evaluated 3 GC treatment strategies for major disease relapse: 1) Standard: prednisone 1 mg/kg daily, tapering to 10 mg daily by month 6, 2) Reduced-dose: prednisone 0.5 mg/kg daily, discontinuing by month 6, and 3) Minimal: varying starting doses, discontinued within 2 months, in conjunction with avacopan. We projected the outcomes of major and minor relapse, incident diabetes mellitus, ≥1 severe infection, end-stage renal disease, and death over 5 years.
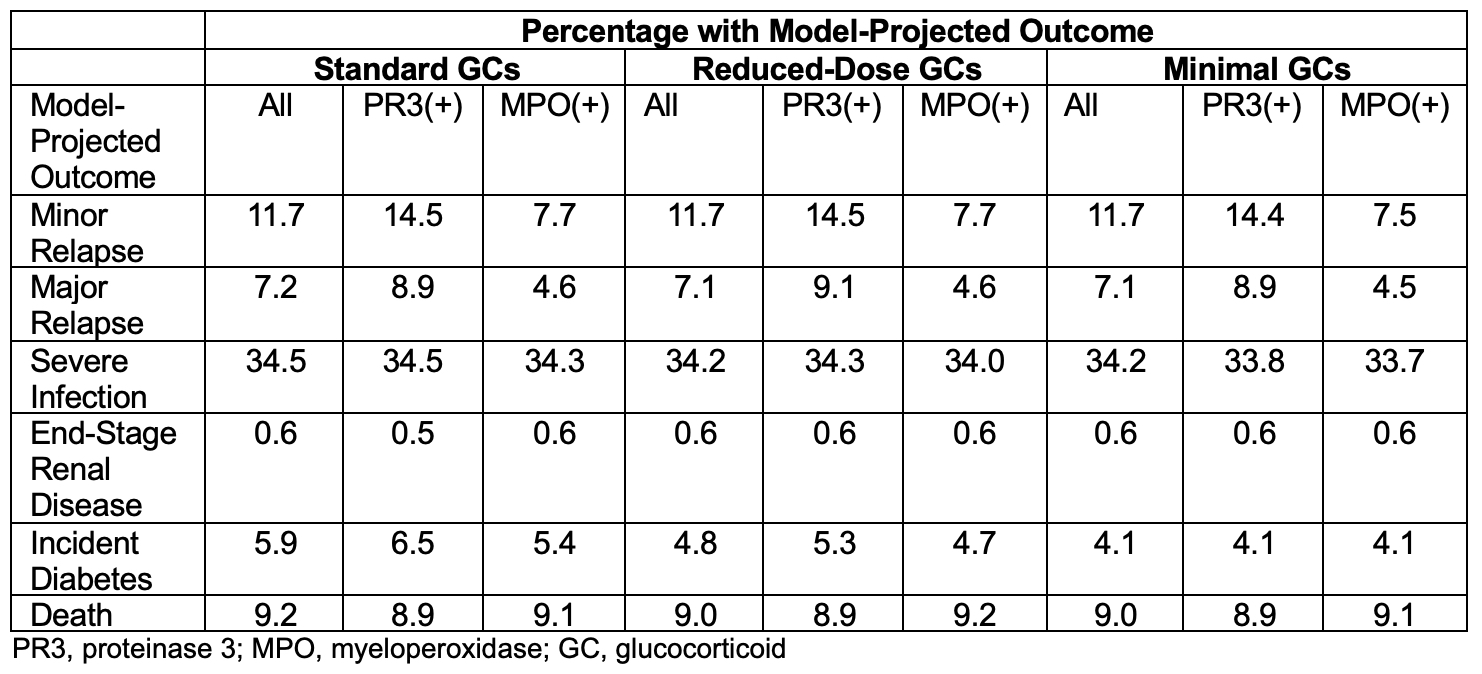
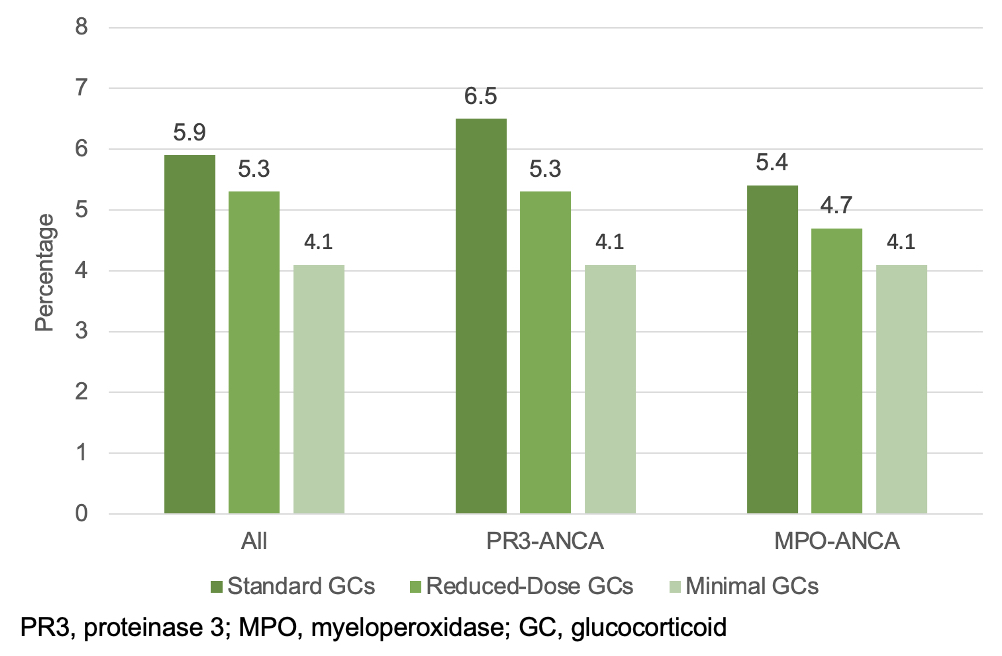
Results: Over 5 years, among all individuals, the projected percentage with incident diabetes (5.9% vs. 4.8% vs. 4.1%) and ≥1 severe infection (34.5% vs. 34.2% vs. 34.2%) would be higher in the standard vs. reduced-dose vs. minimal GC strategies, respectively (Figure; Table 2). Cumulative incidence of death would be slightly higher in the standard GC group (9.2% vs. 9.0% with the other GC regimens). The GC-sparing benefits with regard to diabetes would be greater in PR3 vs. MPO positive individuals (incident diabetes in 6.5% vs. 5.3% vs. 4.1% in PR3 positive versus 5.4% vs. 4.7% vs. 4.1% in MPO positive individuals across GC regimens), owing largely to the greater probability of both major and minor relapse in those with PR3 positivity and subsequent increased GC exposure.
Conclusion: Over 5 years, an AAV treatment strategy that uses minimal GCs would be associated with lower cumulative incidence of diabetes. The GC-sparing benefits would be most notable in people at highest risk of relapse (e.g., PR3-ANCA positivity). These findings highlight the importance of GC-sparing strategies and the need for studies that identify people most likely to benefit.
To cite this abstract in AMA style:
Patel N, Wu A, Srivatsan S, Miloslavsky E, Merkel P, Stone J, Choi H, Hyle E, Wallace Z. Projecting the Impact of Standard, Reduced-Dose, and Minimal-Dose Glucocorticoid Regimens in the Treatment of ANCA-Associated Vasculitis Using Simulation Modeling [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/projecting-the-impact-of-standard-reduced-dose-and-minimal-dose-glucocorticoid-regimens-in-the-treatment-of-anca-associated-vasculitis-using-simulation-modeling/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/projecting-the-impact-of-standard-reduced-dose-and-minimal-dose-glucocorticoid-regimens-in-the-treatment-of-anca-associated-vasculitis-using-simulation-modeling/