Session Information
Date: Monday, October 27, 2025
Title: (1467–1516) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune rheumatic disease with heterogeneous hematologic manifestations. Thrombocytopenia (TP) in SLE may be associated with major organ involvement and poor prognosis. Our study aimed to evaluate the frequency and prognostic significance of TP in a large, single-center SLE cohort.
Methods: We conducted a retrospective cross-sectional study using data from the SLE cohort at University Hospitals Cleveland Medical Center. Patients met 2019 EULAR/ACR classification criteria for SLE. Clinical, demographic, immunologic, and outcome variables were extracted to assess associations with a history of TP, defined as any documented platelet count < 150 × 10⁹/L. Chi-square (χ²) tests were used to assess the relationship between TP and categorical variables, including clinical manifestations, laboratory markers, medication use, and mortality. To determine independent risk factors for TP in SLE patients, multivariate logistic regression analysis was performed. Parameters which were found significant in univariate analysis were utilized in logistic regression analysis. A two-sided p-value of < 0.05 is considered statistically significant. The study was IRB-approved.
Results: Among the 279 SLE patients, 105 (37.6%) had a history of TP. TP was significantly associated with several immunologic and clinical features. Patients with TP were more likely to have leukopenia (74.3% vs. 37.9%, p < .001), lymphopenia (83.8% vs. 36.8%, p < .001), low C3 (41.9% vs. 13.8%, p < .001), and low C4 (37.1% vs. 13.8%, p < .001). There was a non-statistical trend toward higher anti-dsDNA antibody positivity (57.7% vs. 46.5%, p = .072). TP was associated with major organ involvement including increased rates of lupus nephritis (41.0% vs. 18.4%, p < .001), ESRD (21.9% vs. 2.3%, p < .001), CNS involvement (17.1% vs. 9.2%, p = .049), cerebrovascular events (20.0% vs. 4.1%, p < .001), and thrombotic events (25.0% vs. 9.8%, p < .001). Additionally, in this cohort, they had an approximately 6.8-fold higher risk of mortality (7.5% vs. 1.1%, p = 0.039). Use of immunosuppressive therapies, including mycophenolate mofetil (48.6% vs. 26.4%, p < .001) and rituximab (11.4% vs. 3.5%, p = .013), was also significantly more common among patients with TP. In contrast, there were no statistically significant differences between patients with and without TP in terms of gender, race, ethnicity, or comorbid conditions such as hypertension, diabetes mellitus, coronary artery disease, or malignancy. Multivariate logistic regression analysis showed that lymphopenia (OR: 7.6, 95%CI: 1.5-38.5, p=0.014) and the presence of cerebrovascular disease (OR: 37, 95%CI: 2.1-647.2, p=0.013) are independent factors associated with TP in our SLE cohort.
Conclusion: TP in SLE is significantly associated with leukopenia, lymphopenia, and decreased C3/C4. It is also linked to severe clinical manifestations, including lupus nephritis, ESRD, CNS and cerebrovascular events, thrombosis and increased mortality. Multivariate analysis confirmed that lymphopenia and cerebrovascular disease are independent predictors of TP. These findings support TP as a powerful prognostic marker in SLE.
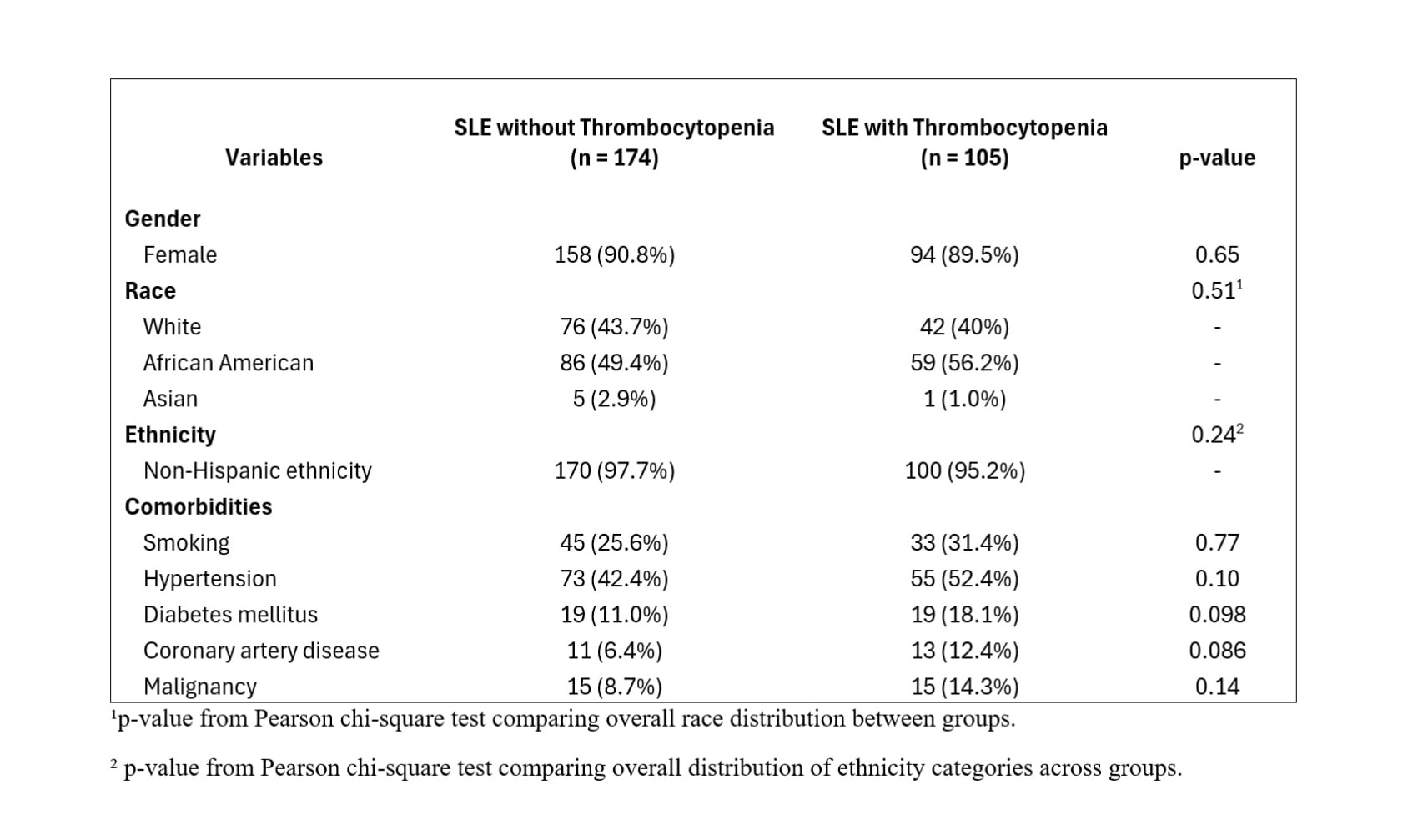 Table 1: Baseline demographics and comorbid conditions in SLE with and without thrombocytopenia.
Table 1: Baseline demographics and comorbid conditions in SLE with and without thrombocytopenia.
.jpg) Table 2: Comparison of serologic markers in SLE patients with and without thrombocytopenia.
Table 2: Comparison of serologic markers in SLE patients with and without thrombocytopenia.
.jpg) Table 3: Clinical manifestation of SLE patients with and without thrombocytopenia.
Table 3: Clinical manifestation of SLE patients with and without thrombocytopenia.
To cite this abstract in AMA style:
Heydari-Kamjani M, Daneshvar A, Nachawati D, Harper E, Pfeil K, Gump M, Frumker L, Pamuk O. Prognostic Impact of Thrombocytopenia on Morbidity and Mortality in Systemic Lupus Erythematosus: A Retrospective Single-Center Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/prognostic-impact-of-thrombocytopenia-on-morbidity-and-mortality-in-systemic-lupus-erythematosus-a-retrospective-single-center-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prognostic-impact-of-thrombocytopenia-on-morbidity-and-mortality-in-systemic-lupus-erythematosus-a-retrospective-single-center-study/
