Session Information
Date: Sunday, November 13, 2022
Title: SLE – Treatment Poster II
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: To compare use of autoimmune disease treatments between patients with and without severe COVID-19 (COVID) in cohorts of patients with systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), or myositis (MYO).
Methods: Healthcare claims in the IBM® MarketScan® Commercial Database were used to identify adults (18+) with a confirmed diagnosis of SLE, RA, or MYO between 1/1/2013 and 4/1/2020. Observation began on 4/1/2020 and ended with the earliest of enrollment end, death, or 12/31/2021. Severe COVID was identified as an inpatient (IP) claim with a COVID ICD-10 diagnosis code (U071 or J1282). Use of antimalarials, biologics, and immunosuppressants was assessed in the 6 months before a patient’s earliest COVID diagnosis, and corticosteroid use was assessed in the prior 30 days. For patients without severe COVID, medication use was assessed in the 6 months (or 30 days) before a proxy date, assigned based on a matched distribution of earliest diagnosis dates among patients with severe COVID. Medication use was not assessed for 17% of SLE patients without severe COVID whose assigned proxy date was outside of their observation period. Demographics were assessed on 4/1/2020. SLE disease severity and diagnoses in the Elixhauser Comorbidity Index were assessed among patients enrolled during the 12 months before 4/1/2020. Unadjusted comparisons between patients with and without severe COVID were made with chi-square or Fisher’s exact tests.
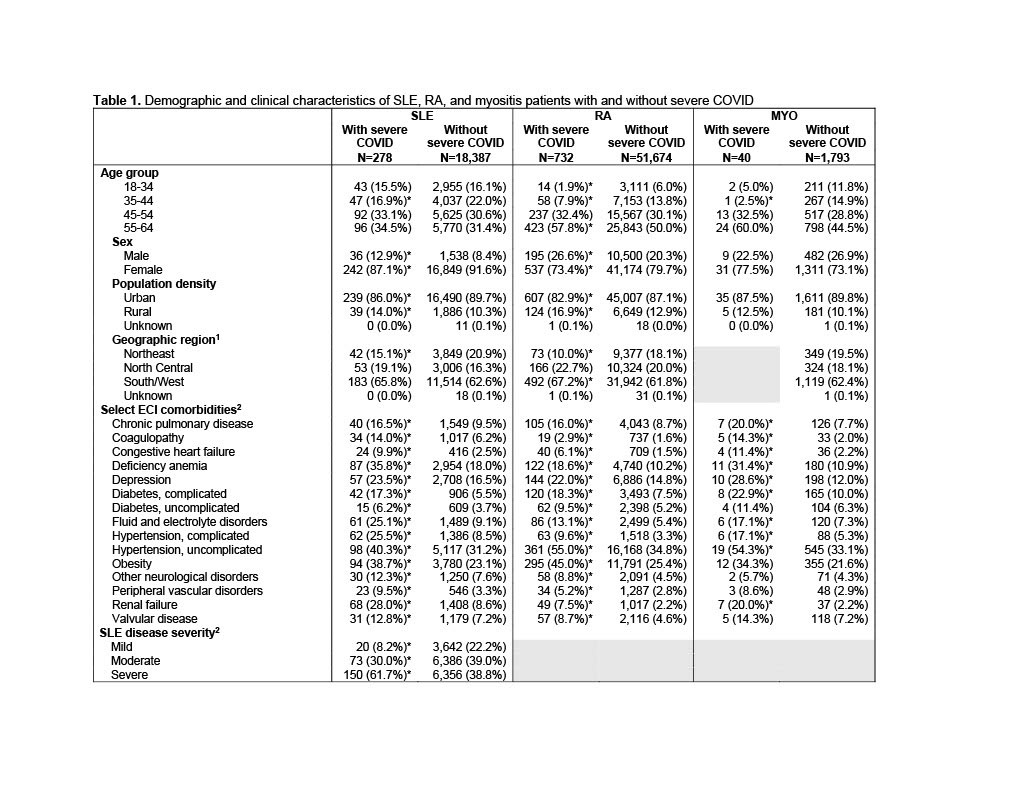
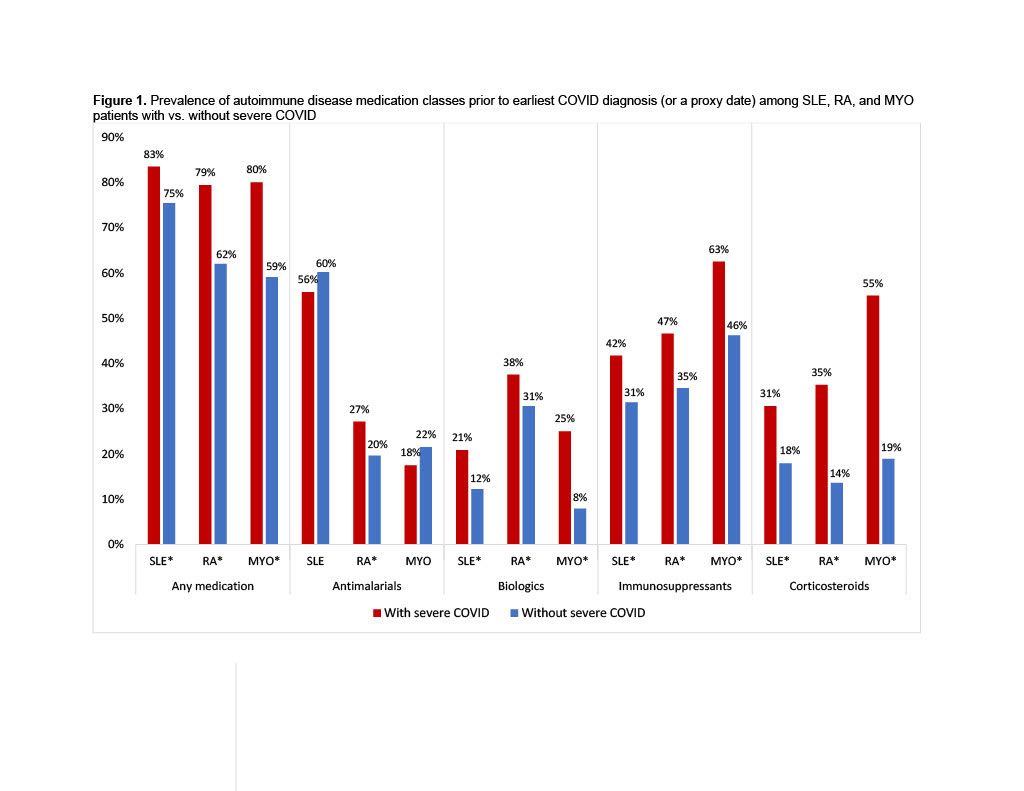
Results: 18,665 patients with SLE, 52,406 with RA, and 1,833 with MYO met inclusion criteria. Severe COVID occurred among 1.5% of SLE, 1.4% of RA, 2.2% of MYO patients. Patients with severe COVID were older in all three cohorts, and SLE and RA patients with severe COVID were more likely to be male, compared to patients without severe COVID (Table 1). Comorbidities were significantly more common among patients with severe COVID in all three cohorts. Patients with severe COVID in each disease cohort were significantly more likely to have previously used any medication (79-83%), compared to patients without severe COVID (62-75%) (Figure 1). Prior use of any biologic, immunosuppressant, or corticosteroid was also significantly more common among patients with severe COVID in each cohort, and use of antimalarials was more common among RA patients with severe COVID. SLE, RA, and MYO patients with severe COVID were more likely to have used rituximab (7-20%) or mycophenolate (3-40%), compared to patients without severe COVID (2-6% and 1-15%, respectively) (Figure 2). Belimumab was more common among SLE patients with vs. without severe COVID (12% vs. 8%), and leflunomide and tacrolimus were more common among SLE and RA patients with vs. without severe COVID (SLE: 4% vs. 2% and 8% vs. 3%; RA: 12% vs. 6% and 1% vs. 0.3%). No use of anifrolumab was found in the 6-months before severe COVID events.
Conclusion: Some autoimmune disease treatments especially corticosteroids, are more prevalent among SLE, RA, and MYO patients with severe COVID. These treatments may be indicative of autoimmune disease severity, or independently associated with the occurrence of severe COVID. The potential impact on patients’ COVID risk should be carefully considered when selecting or adjusting autoimmune treatment regimens.
To cite this abstract in AMA style:
Calabrese C, Atefi G, Evans K, Moynihan M, Palmer L, Wu S. Prior Use of Autoimmune Disease Treatments Among Patients with Systemic Lupus Erythematosus, Rheumatoid Arthritis, or Myositis Hospitalized with COVID-19 [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/prior-use-of-autoimmune-disease-treatments-among-patients-with-systemic-lupus-erythematosus-rheumatoid-arthritis-or-myositis-hospitalized-with-covid-19/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prior-use-of-autoimmune-disease-treatments-among-patients-with-systemic-lupus-erythematosus-rheumatoid-arthritis-or-myositis-hospitalized-with-covid-19/