Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Osteoporosis (OSP) is common, carries high morbidity, significant cost and remains underrecognized and undertreated by health care providers (1). At a university-based academic health system in Southern California, a Fracture Liaison Service (FLS) has been established to ensure secondary prevention. A dedicated OSP clinic was established in 2018. OSP specialists regularly provide education and collaboration with PCPs and IM residents rotate through a two-week OSP rotation. It would be expected that primary prevention (PP) of OSP fractures be higher than the national rate of ≈ 16% (2). The objective of this study is to examine how PP of fragility fractures is addressed in an academic health system with a dedicated OSP treatment and education team.
Methods: The outpatient electronic medical records of adults who qualified for OSP treatment based on FRAX score or T score between January and May 2022 were reviewed. Basic demographic information was noted. Patients with prior OSP fracture were excluded. The medical specialty of the physician referring for BMD testing was noted. Whether the patient was offered treatment was noted as were rates of treatment acceptance.
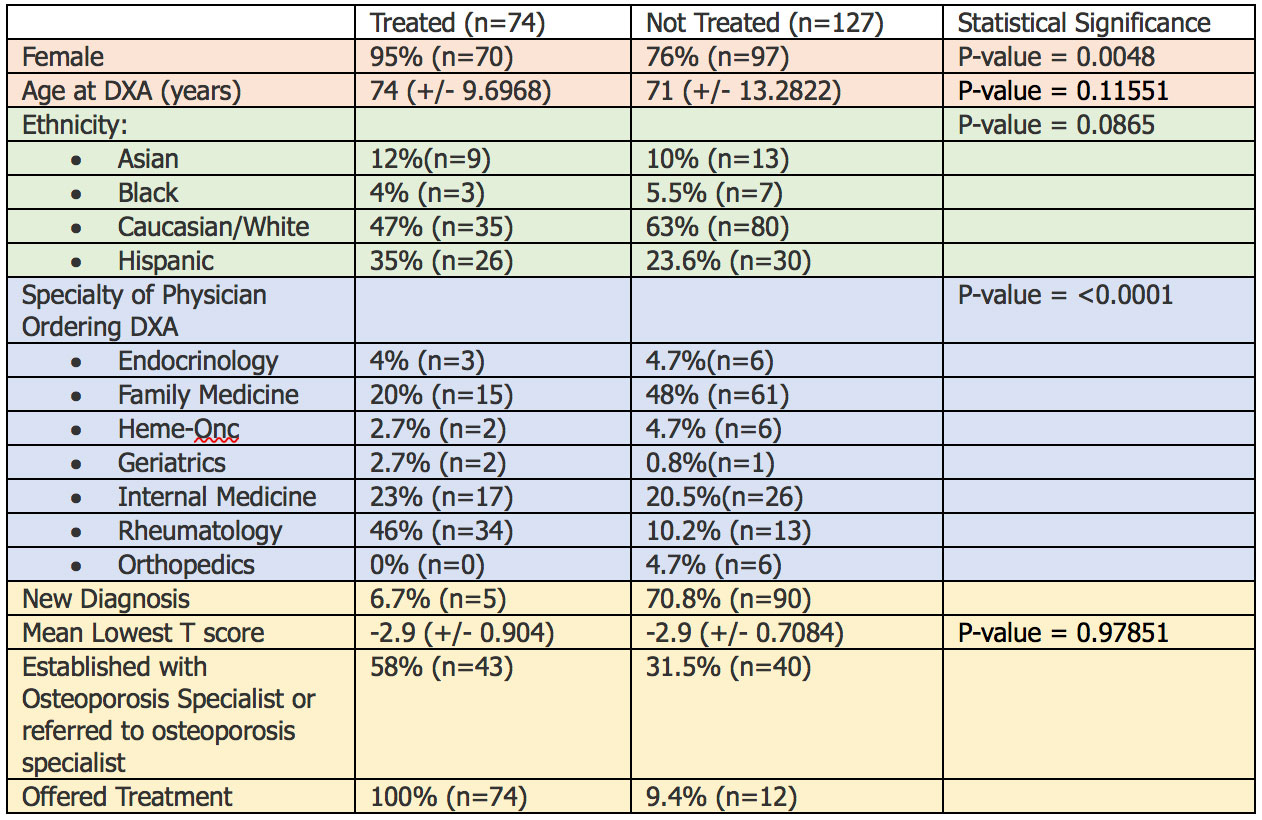
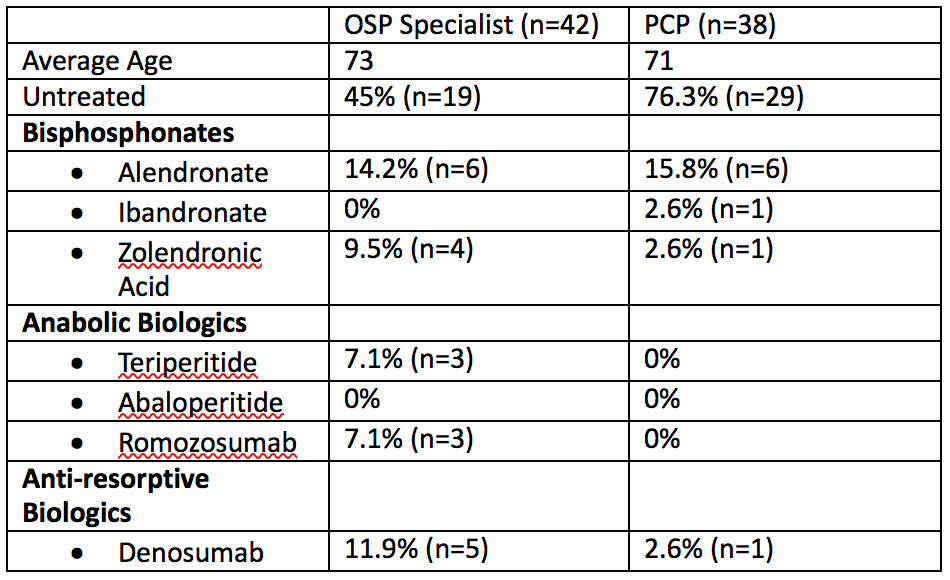
Results: 201 patient charts were reviewed, all qualifying for treatment. Seventy-four patients (37%) were on OSP treatment at time of chart review and 127 (63%) weren’t (Table 1). Differences between groups in age, ethnicity and lowest T score were not significant. For most untreated patients (70.8%) the DXA was not the first showing OSP. Rheumatologists were most likely to treat patients for OSP (46% of providers) and more likely to use biologics for severe OSP (Table 2). Almost half of the ordering physicians who did not treat when required were Family Medicine (48%). 58% of the patients who were treated were seen in the OSP clinic. 31.5% were seen in the OSP clinic but not treated. Only 9.4% of the untreated patients were offered treatment according to documented clinical notes.
Conclusion: This is an ongoing study. PP at our academic center surpassed the national average by 21%. Given the relatively higher rates of treatment in those either cared for by an OSP clinic or rheumatology, having access to providers with OSP experience is beneficial for patients. Significant care gaps remain. Areas of further study include determining reasons for not treating, including investigating PCP comfort with biologic use in OSP. The fact that 31.5% of untreated patients who were seen by an OSP specialist were not treated points toward treatment refusal rather than offering. Documentation of offering treatment in the notes may be lacking. Availability of OSP specialists increases primary prevention in OSP.
References
- Kanis, John A., et al. “The Osteoporosis Treatment Gap.” Journal of Bone and Mineral Research, vol. 29, no. 9, 2014, pp. 1926–28. doi:10.1002/jbmr.2202
- Weaver, Jessica, et al. “Diagnosis and Treatment of Osteoporosis Before and After Fracture: A Side-by-Side Analysis of Commercially Insured and Medicare Advantage Osteoporosis Patients.” Journal of Managed Care & Specialty Pharmacy, vol. 23, no. 7, 2017, pp. 735–44. doi:10.18553/jmcp.2017.23.7.735
To cite this abstract in AMA style:
Looi E, Mishkova G, Downey C. Primary Prevention of Fractures in Osteoporotic Patients in a Southern California Academic Health System [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/primary-prevention-of-fractures-in-osteoporotic-patients-in-a-southern-california-academic-health-system/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/primary-prevention-of-fractures-in-osteoporotic-patients-in-a-southern-california-academic-health-system/