Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Musculoskeletal ultrasound is an important imaging method in the diagnosis of arthritis, especially rheumatoid arthritis (RA). The prevalence of elbow joint arthritis in RA has not yet been specifically investigated sonographically and correlated with the clinical examination and other parameters.
Methods: In 100 patients with RA and 50 patients without rheumatological disease both cubital joints were examined according to the 3 most relevant standard planes (anterior longitudinal humeroradial and humeroulnar as well as posterior longitudinal scans) of the German Society for Ultrasound in Medicine (DEGUM). A complete clinical examination was performed and baseline characteristics (age, sex, etc.), DAS28 and visual analogue scale (VAS) were recorded. Elbow arthritis was defined as joint effusion grade II and/or hyperperfusion of the synovial proliferation. The patients were recruited in the department of Rheumatology of the University Hospital Bonn as well as in the Rheinischen Rheumazentrum Meerbusch. The ultrasound examination was performed by two very experienced physicans (DEGUM level I and DEGUM level II, equals EFSUMB levels). The statistical evaluation was performed with IBM SPSS (Version 25). A p-value < 0.05 was considered significant. The interrater analysis was assesed by Cohen’s kappa, as well as by an independent blinded assessor (DEGUM III, equal EFSUMB III).
Results: Mean age was 59.8 years (±SD 15.9) in the RA cohort and 59.8 years (±SD 16.2) in the control group. The RA cohort displayed relevant joint effusion in 54.9%, in 6.9% hypervascularization was visible, whereas in the control group 16% displayed joint effusion and none showed hypervascularization. The mean DAS28 in the RA cohort was 5.3 (±SD 1.1; high activity 56.9% (DAS28 > 5.1), moderate activity 41.1% (DAS28 > 3.2), low activity (DAS28 > 2.6) 2%). The mean VAS in RA patients was 6.41 (±SD 2.3), and 2.42 (± 2.9) in the control group.
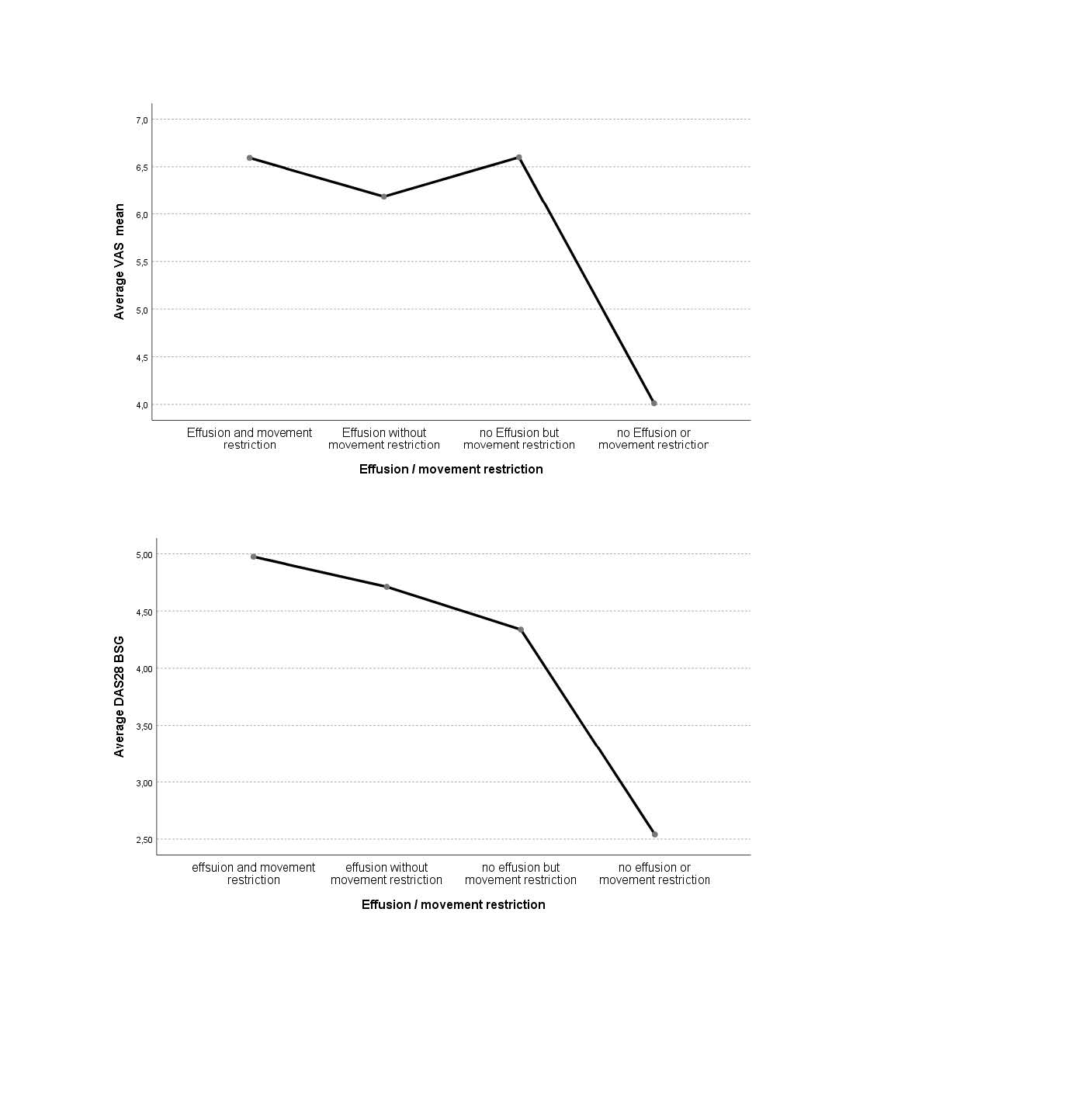
In the RA cohort there was a significant correlation between movement restriction (MR) and joint effusion (p-value = 0.001), between DAS28 and MR (p-value = 0.02) and between DAS28 and sonographic joint effusion (p-value = 0.022). The overall collective showed a significant correlation of DAS28 with MR and joint effusion [figure 1].
In overall analysis, a highly significant correlation of VAS with MR (p-value 0.001), the presence of joint effusion (p-value 0.001) and the diagnosis of RA (p-value 0.001) was observed.
Interrater analysis showed good agreement with Cohen´s kappa of 0,896 and a highly significant p-value of 0.001.
Conclusion: This is the first study to investigate the prevalence of elbow joint effusion and synovitis in RA patients. It shows, that the prevalence of elbow joint arthritis is high, with over 54% in the RA cohort. Movement restriction is a good indicator of elbow joint arthritis in RA, but not in all RA patients. In the overall analysis of both cohorts, there is a strong correlation between VAS with joint effusion and MR (p-value 0.001) [Figure 2].
To cite this abstract in AMA style:
Vossen D, Schaefer V, Recker F, Geffken I, Matuschek E, Hartung W. Prevalence of Elbow Arthritis in Patients with Rheumatoid Arthritis: A Prospective Ultrasound Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-elbow-arthritis-in-patients-with-rheumatoid-arthritis-a-prospective-ultrasound-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-elbow-arthritis-in-patients-with-rheumatoid-arthritis-a-prospective-ultrasound-study/