Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Familial aggregation of autoimmune disease as well as co-occurrence of multiple autoimmune diseases in one individual is known and it suggests a shared genetic basis for autoimmunity. Though there is significant data available on familial aggregation of autoimmune diseases in adult rheumatic diseases, the data in JIA is limited1,2 and is scant from South Asia. In South Asia, enthesitis related arthritis (ERA) is the commonest category of JIA. We looked at the prevalence of autoimmune diseases among family members of children with JIA.
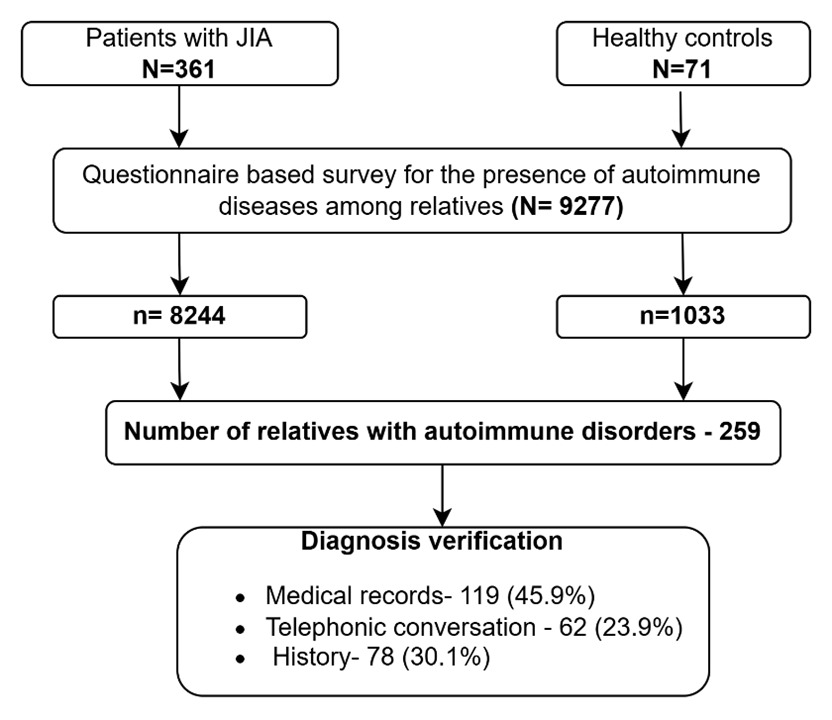
Methods: Families of patients with JIA who satisfied the ILAR classification criteria for JIA were enrolled in the study after obtaining a written informed consent. They were asked about the history of autoimmune diseases in the patient as well as among the first, second and third degree relatives, with the help of a questionnaire. The presence of autoimmune disease was confirmed from medical records, prescriptions or telephonic conversations with patients or relatives where ever possible (Figure 1).
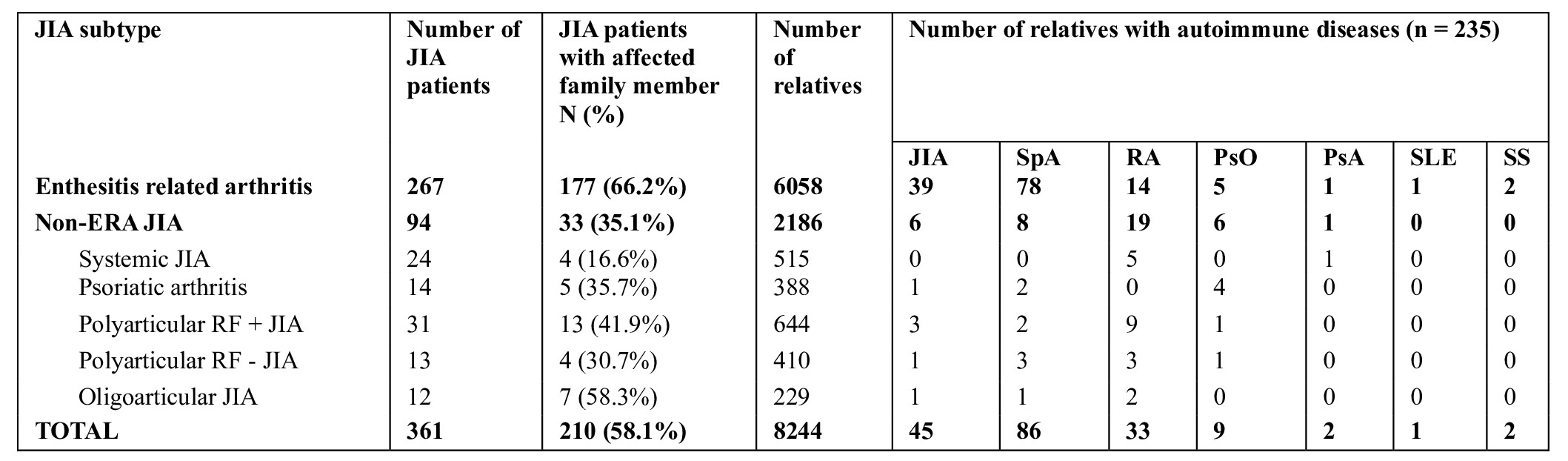
Results: 8244 relatives of 361 patients with JIA (median age of 18 years, duration of disease 6 years, JADAS 7.95; 280 males) and 1033 relatives of 71 healthy children were included in the study. There were more female relatives in both groups. The distribution of JIA categories was: 267 ERA, 31 polyarticular RF+ JIA, 24 sJIA, 14 psoriatic arthritis, 13 polyarticular RF negative JIA and 12 oligoarticular JIA (Table 1). Seven (1.93%) JIA patients had another coexisting autoimmune disease.
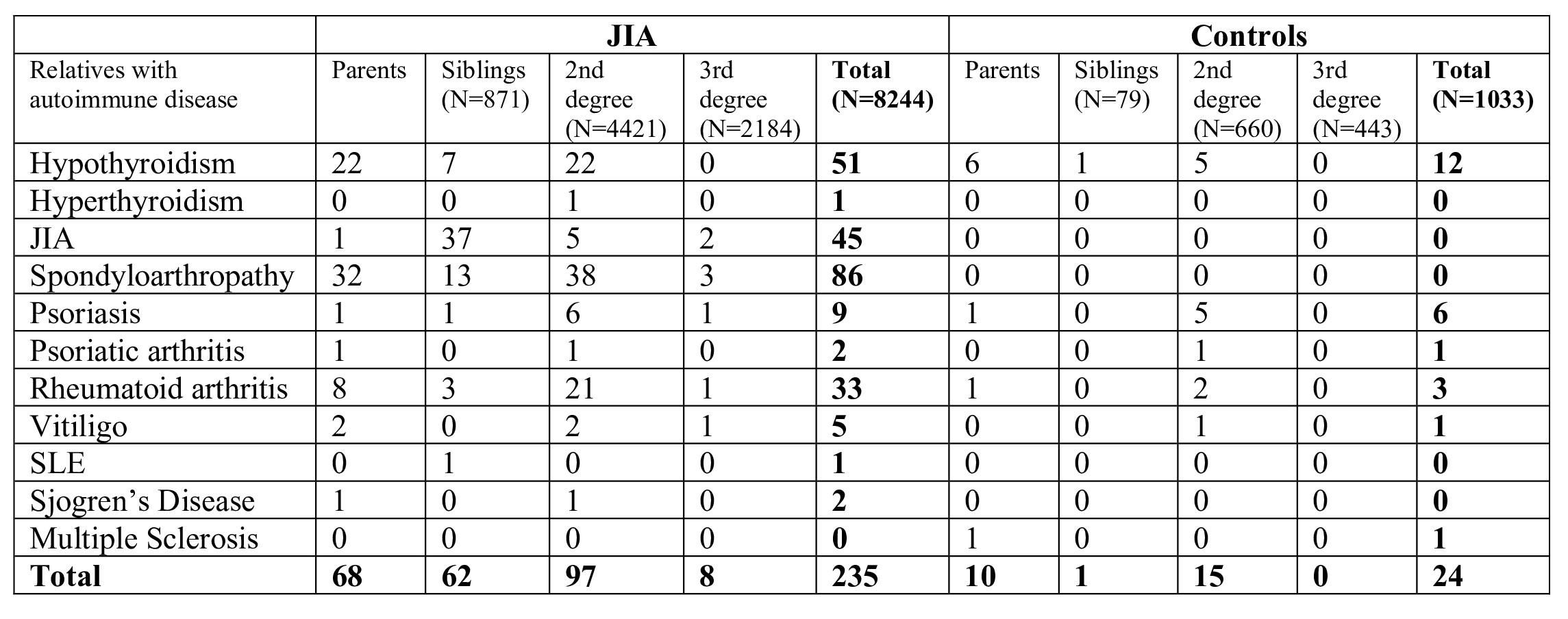
210 (58%) children with JIA had at least one relative with an autoimmune disease whereas among healthy children, 15 (22.5 %) had a relative with autoimmune disease (p< 0.001). The proportion of patients with positive family history varied from 16 to 66% in different categories of JIA. (Table 1) Spondyloarthropathy & JIA were the common autoimmune disease among relatives of JIA patients especially so in children with ERA. In non-ERA hypothyroidism followed by RA were common. (Table 1)
The prevalence of autoimmune disease was higher in first degree relatives as compared to second degree relatives (130/1639 versus 97/4421; p< 0.001). Among JIA, 2.5% maternal relatives had an autoimmune disease as opposed to 1.9% paternal relatives (p< 0.001). There was a higher prevalence of spondyloarthropathy among paternal relatives as compared to maternal relatives (1.1% versus 0.7%. p< 0.05). The prevalence of autoimmune diseases among maternal and paternal relatives of controls were 2.3% and 1.2% respectively.
Conclusion: More than half of the children with JIA have family members with autoimmune disease suggesting shared genetic basis of JIA. Screening of relatives of JIA may help in early recognition of autoimmune disease in community.
To cite this abstract in AMA style:
Minikumari Rahulan L, Lawrence A, Aggarwal A. Prevalence of Autoimmune Diseases in 8244 Family Members of Children with Juvenile Idiopathic Arthritis: A Study from India [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-autoimmune-diseases-in-8244-family-members-of-children-with-juvenile-idiopathic-arthritis-a-study-from-india/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-autoimmune-diseases-in-8244-family-members-of-children-with-juvenile-idiopathic-arthritis-a-study-from-india/