Session Information
Date: Saturday, November 6, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster I (0387–0413)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: To study the prevalence, anatomical distribution, clinical correlates and outcomes of macrovascular disease (MVD) on duplex ultrasound (US) of the upper extremity in Systemic sclerosis (SSc) patients evaluated at a single tertiary referral center.
Methods: Medical records of SSc patients meeting ACR/EULAR 2013 classification criteria that underwent upper extremity duplex US with laser doppler flowmetry between Jan 2001-Dec 2018 at our institution were retrospectively reviewed to abstract the presence or absence of MVD (stenosis/occlusion involving the palmar arch, ulnar, radial, brachial, axillary and/or subclavian arteries). Demographics, clinical characteristics, and outcomes were abstracted to evaluate risk factors associated with MVD in SSc and its association with digital ischemic complications. Logistic regression models were adjusted for age at vascular study and gender.
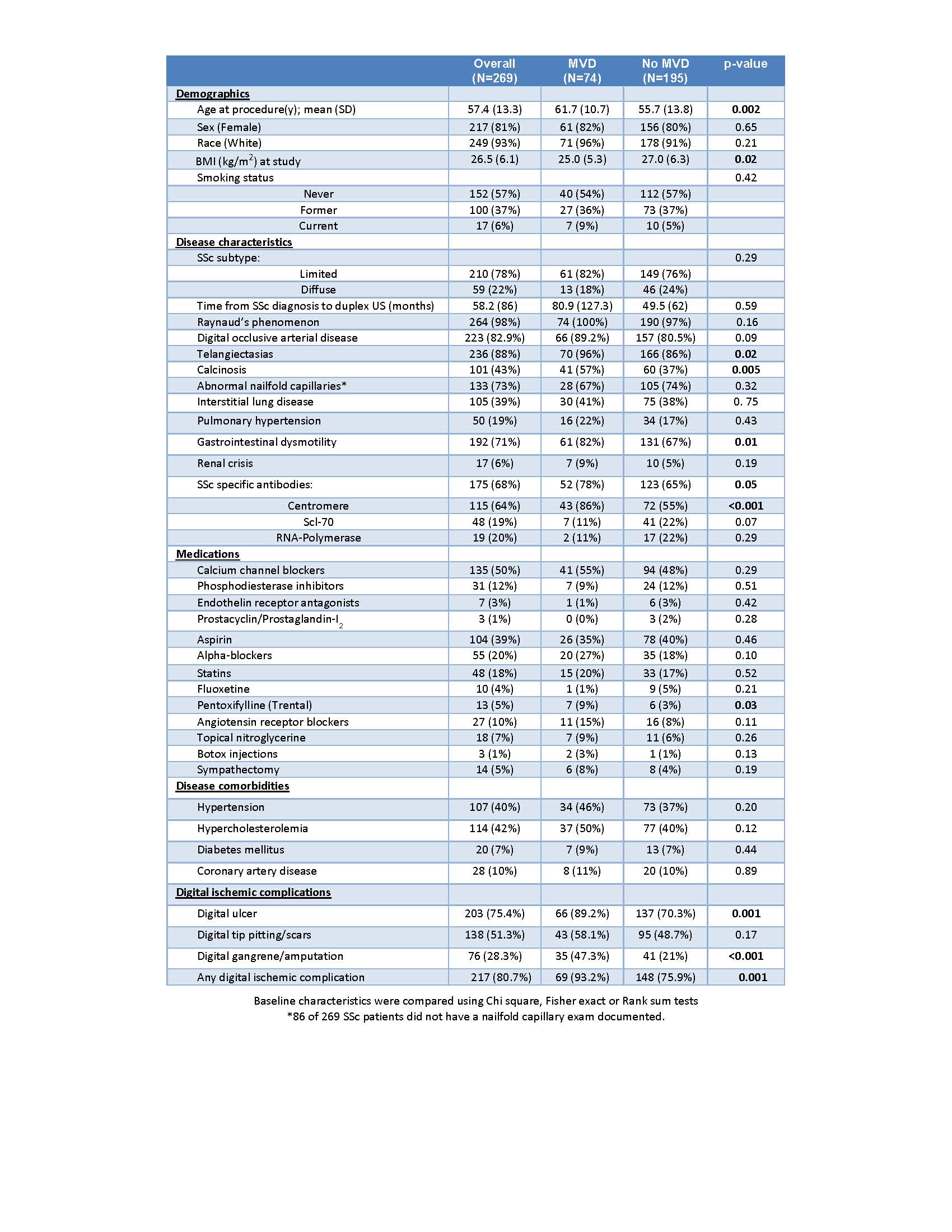
Results: 269 SSc patients (mean age 57.4 ± 13.3 y, 81% female, 93% Caucasian) underwent upper extremity duplex US during the study period. Mean disease duration was 4.8 ± 7.2 y. The majority had limited cutaneous SSc (lcSSc) (78%) and 68% had a positive SSc specific antibody. Cohort characteristics are described in Table 1.
Macrovascular arterial disease was prevalent at the time of duplex US in 74 patients (28%; bilateral in 13%): Ulnar occlusive disease was the most common, noted in 68 patients (25%; bilateral in 11%) followed by radial in 14 (5%), palmar arch in 6 (2%) and subclavian in 4 (1%). No patients had brachial or axillary artery involvement.
SSc patients with MVD were compared to those without MVD, and were noted to have a significantly higher prevalence of centromere pattern-ANA (86% vs 55%, p < 0.001), older age (61.7 vs 55.7 y, p=0.002), calcinosis (57% vs 37%, p= 0.005), telangiectasias (96% vs 85%, p=0.02) and GI dysmotility (82% vs 67%, p=0.01). Mean BMI was lower among those with MVD (25 vs 27, p=0.02). Digital occlusive arterial disease (defined as pre- and post-warming blood flow of ≤206 arbitrary units on laser doppler flowmetry) was higher among those with MVD (89.2% vs 80.5%, p=0.09), but did not reach significance. There was no difference in skin sclerosis, nailfold capillary abnormalities, ILD, PAH, renal crisis, cardiac involvement, inflammatory arthritis and myositis among SSc patients with and without MVD.
Patients with MVD had a significantly higher odds of having any digital ischemic complications (digital ulcers, pitting scars, gangrene, amputation) than those without MVD (93.2% vs 75.9%, OR 4.99, p =0.001) (Table 2). The odds of certain digital ischemic complications were even higher among those with bilateral MVD than unilateral or no MVD as shown.
Conclusion: In this largest single center cohort of SSc patients assessed with duplex US, more than 1 in 4 patients had MVD. Ulnar occlusive disease was most common, followed by radial arterial disease. Presence of MVD increased the odds of developing digital ischemic complications 4 to 5-fold among patients with SSc. This study highlights the high prevalence of MVD in SSc, and need to consider aggressive therapeutic intervention in those with MVD to prevent digital ischemic complications.
To cite this abstract in AMA style:
Makol A, Coffey C, Gunderson T, Hinze A, Radwan Y, Crowson C, Liedl D, Warrington K, Wennberg P. Prevalence, Distribution, Clinical Correlates and Outcomes of Upper Extremity Macrovascular Disease in Systemic Sclerosis: Results from a Single Center Referral Cohort (2001-2018) [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/prevalence-distribution-clinical-correlates-and-outcomes-of-upper-extremity-macrovascular-disease-in-systemic-sclerosis-results-from-a-single-center-referral-cohort-2001-2018/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-distribution-clinical-correlates-and-outcomes-of-upper-extremity-macrovascular-disease-in-systemic-sclerosis-results-from-a-single-center-referral-cohort-2001-2018/