Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: PMR, a common inflammatory rheumatic disease in older adults, is primarily treated with glucocorticoids (GC). A high comorbidity burden in PMR may increase the risk of GC toxicity. Frailty, characterized by poor health outcomes and increased vulnerability to stressors is more frequent in PMR (17%)1 than in community dwelling elderly (11%)2. There are limited data on the prevalence of patients with PMR and comorbidities or frailty that may warrant more personalized PMR management (earlier specialist care, screening, lower GC dose/faster taper). Here, we describe the prevalence and management of comorbidities, resulting from or worsening due to long-term GC use, and frailty in PMR.
Methods: Patients aged ≥50 years, without PMR or GCA history, ≥1 inpatient or ≥2 outpatient PMR ≥30–< 365 days apart were identified from Medicare claims from 10/1/2016 to 12/31/2019. Initial GC (prednisone equivalent) use had to be 7.5–25 mg/day ≤30 days after 1st inpatient code or from 1st outpatient to ≤30 days after 2nd outpatient code, ≥200 mg in first ≤30 days and continuous ≥ 4 months. Patients with seropositive RA, other systemic rheumatic disease, organ transplant, multiple sclerosis, active malignancy treatment or prescription for methotrexate, leflunomide, azathioprine or IL-6 receptor inhibitor during baseline were excluded.
We report the prevalence of comorbidities (based on diagnosis, procedure or drug codes) that might be relative contraindications to long term GC use and frailty (assessed with a validated claims-based frailty index [CFI]3; defined as CFI ≥0.24), GC use, care by rheumatology, and screening with DXA.
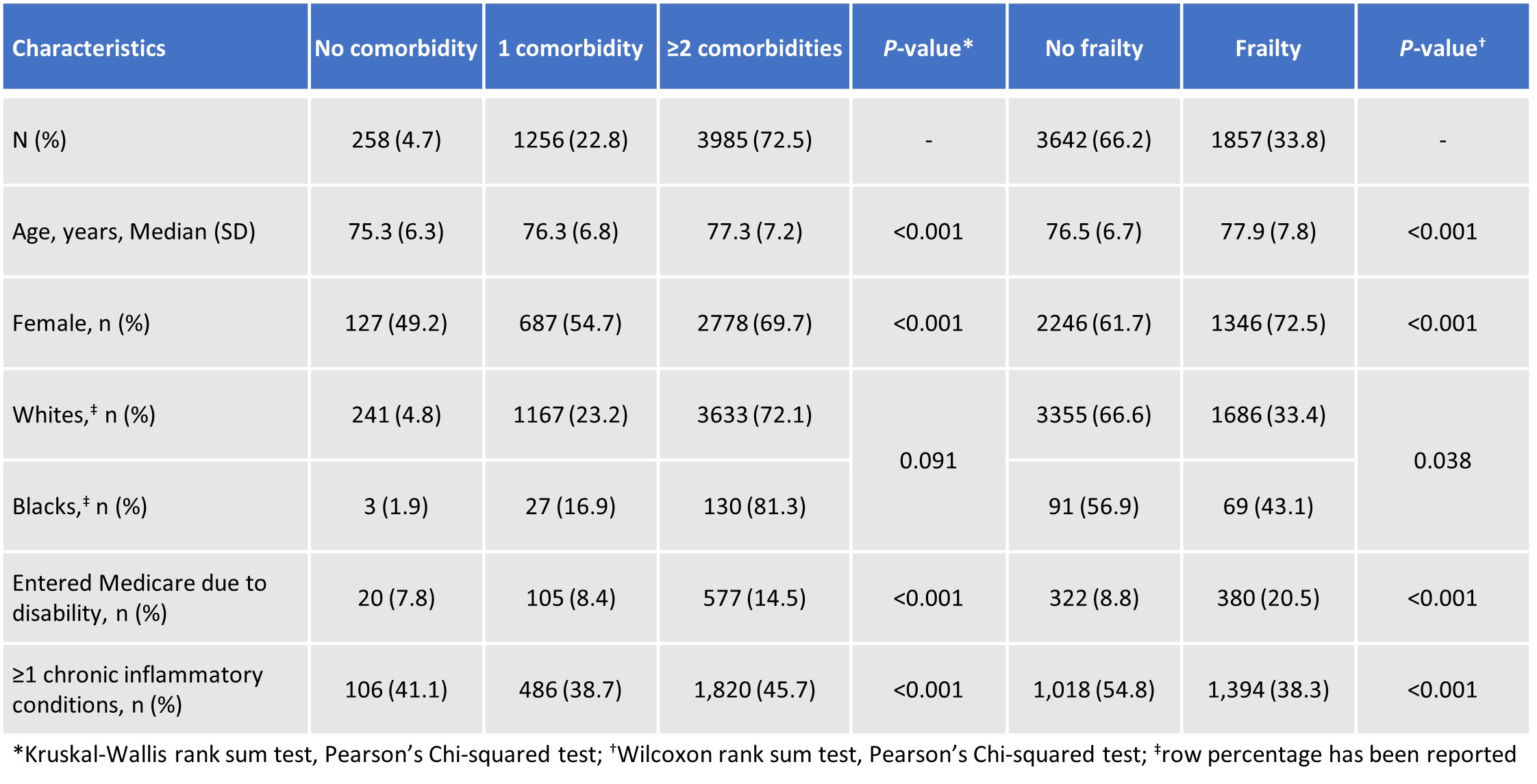
Results: Of 5,499 patients with new onset PMR, at baseline 4.7%, 22.8% and 72.5%, had no, 1 and ≥2 comorbidities, respectively and frailty was seen in 33.8% (Table 1).
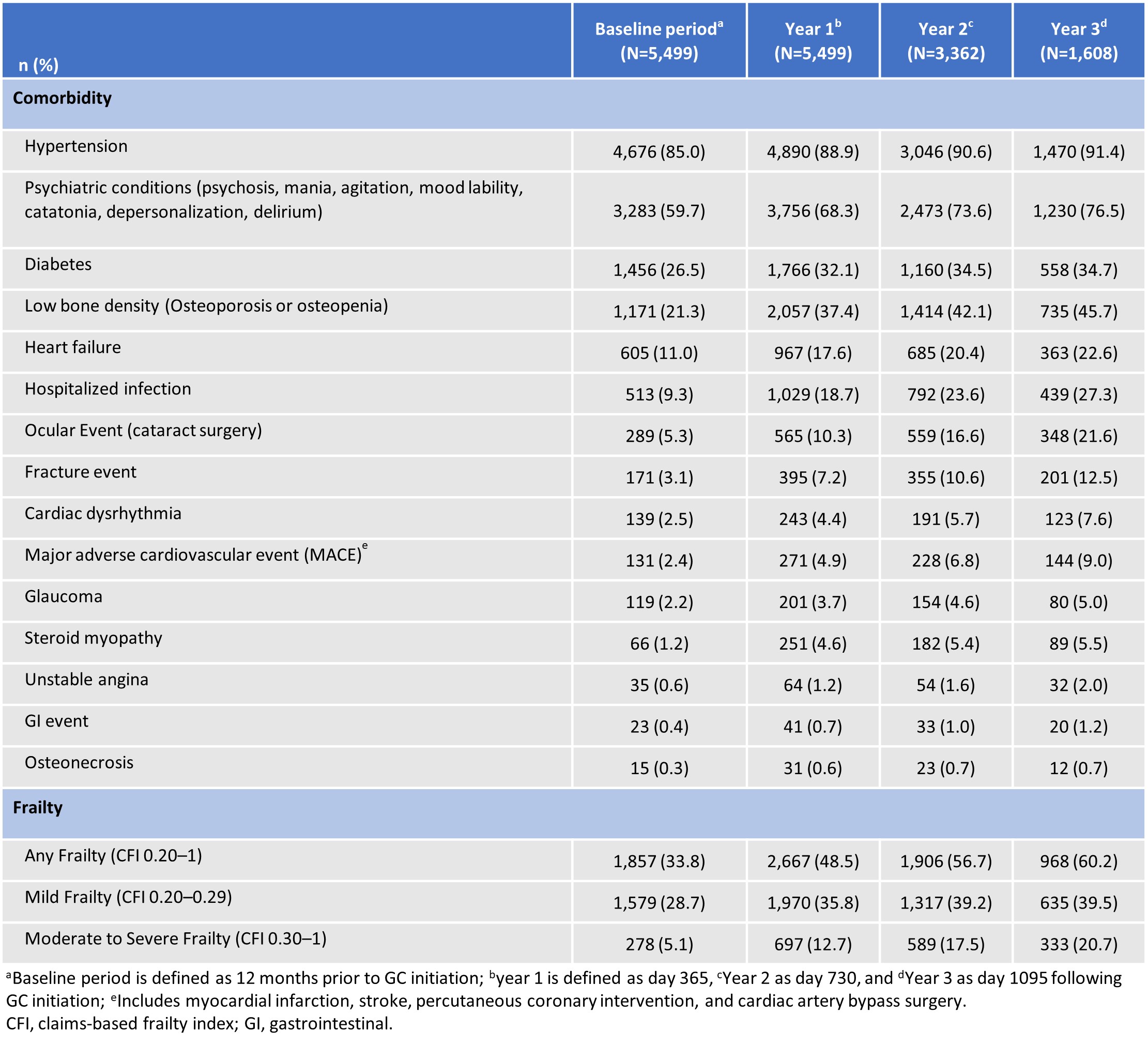
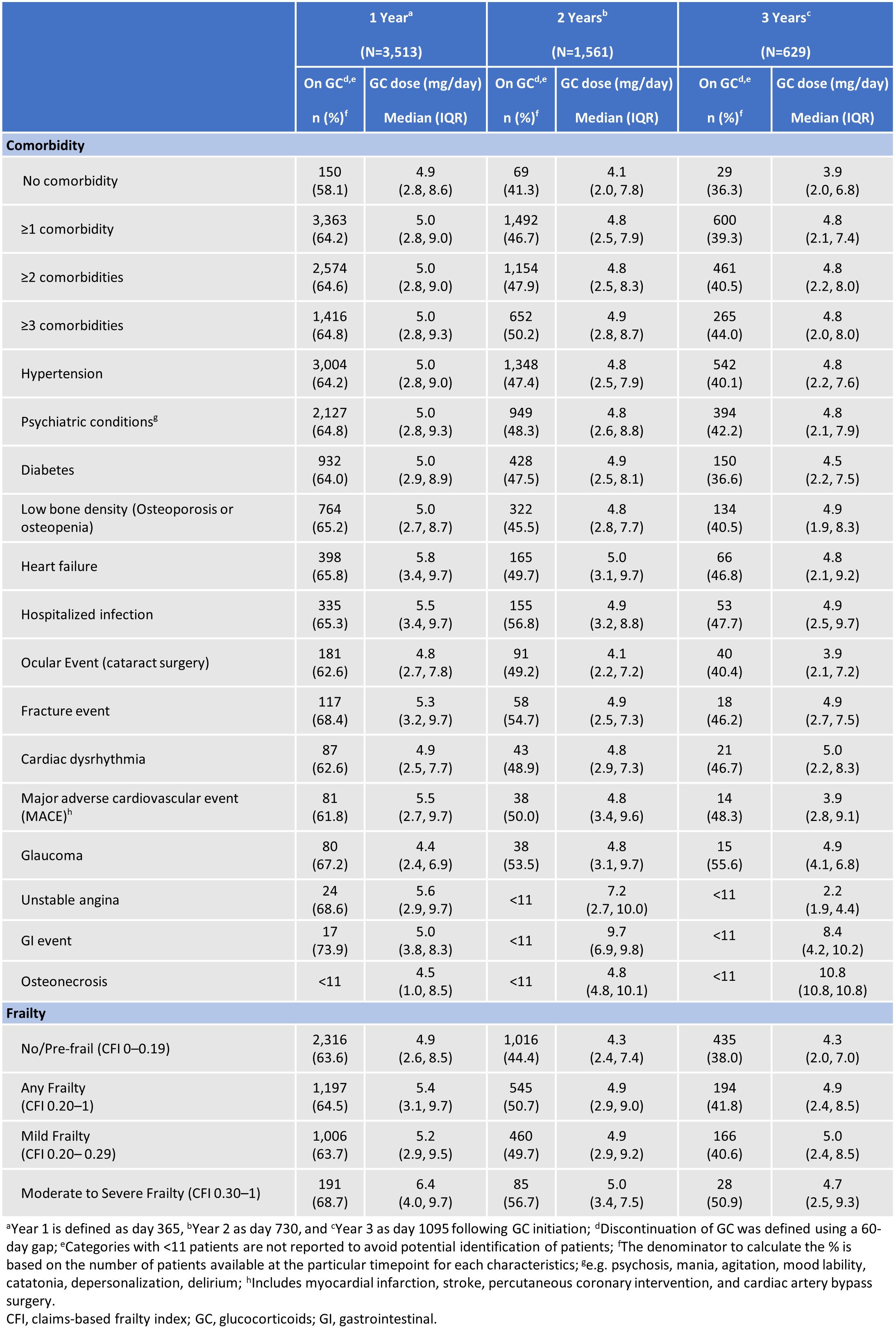
Comorbidities and frailty increased over 3 years, with a 4-fold increase in moderate-severe frailty (Table 2). Patients with a higher burden of comorbidities and who were frail were more likely to be on long term GCs (Table 3).
DXA was obtained ≤2 years prior to GC use to ≤3 months after in 42.8%, 72.4%, 56.7%, and 35.6% of all patients, those with low BMD, those with fracture (other comorbidities range: 24.4%–49.6%) and those with moderate-severe frailty, respectively. Although 57.4% of PMR patients visited rheumatology within the first 6 months, 36.7% did not in ≤3 years. Rheumatology consultations for PMR were similar regardless of comorbidity or frailty.
Conclusion: Many new onset PMR patients had or developed comorbidities and frailty over 3 years, possibly due to GC, PMR activity, aging or other factors. Frailty was higher than previously reported in PMR and community dwelling elderly patients. Despite increased vulnerability to GC toxicity, no substantial difference was observed in GC use in frail patients, possibly due to lack of highly effective alternative treatments. Additional measures are needed to improve access to rheumatology care and BMD screening in patients with PMR.
References:
-
Sattui SE, et al. Rheumatology (Oxford). 2022
-
Collart RM, et al. J Am Geriatr Soc. 2012
-
Halawa OA, et al. Ophthalmology. 2023
-
Kim DH, et al. J Gerontol A Biol Sci Med Sci. 2018
Original presentation: EULAR 2024
To cite this abstract in AMA style:
Sattui S, DR. BUTTGEREIT F, Lidar M, Ford K, Fiore S, Araujo L, Beukelman T, Xie F, Curtis J. Prevalence and Management of Patients with Comorbidities and Frailty in New Onset Polymyalgia Rheumatica [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-management-of-patients-with-comorbidities-and-frailty-in-new-onset-polymyalgia-rheumatica/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-management-of-patients-with-comorbidities-and-frailty-in-new-onset-polymyalgia-rheumatica/