Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: SSc patients have high disability and low quality of life (QoL), driven partially by poor physical function (PF), Gastro Intestinal (GI) problems, digital ulcers (DUs), and pain. The immune driven involvement of peripheral nerves has been identified as an understudied pathogenic step in key SSc manifestations, including Raynaud’s and GI involvement. On the contrary, the role of Peripheral Neuropathy (PN) in diabetes related manifestations including skin ulcers is well understood, mainly from lower limb studies and it has been suggested as potential surrogate marker for GI involvement, including gastroparesis[1]
Here we aim to build on the knowledge from diabetes and detect PN in a large SSc patient cohort, to start and dissect its role in the impact of SSc to patients’ lives.
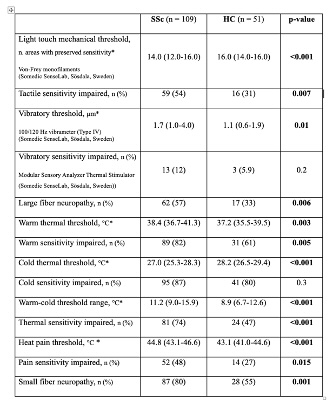
Methods: SSc patients and healthy controls (HC) comparable for age and gender, were enrolled in a cross-sectional observational case-control study. They underwent a detailed quantitative sensory testing of feet evaluating touch, vibratory, thermal, and pain sensitivity; investigating the presence of large and small fiber neuropathy. Neuropathic symptoms were assessed through numerical rating scales, and their impact through patient-reported outcomes on disability and QoL.
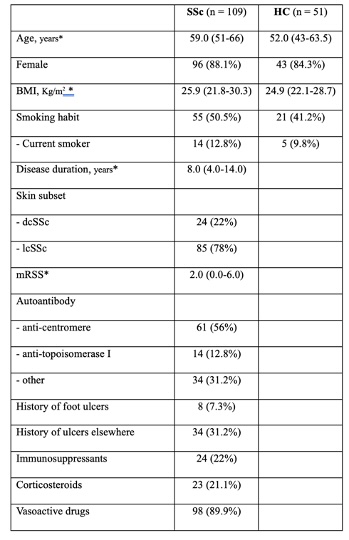
Results: 109 SSc patients (88.1% female, median age 59.0 years) and 51 HC were enrolled (table 1). SSc patients presented with a significant impairment in each sensory parameter assessed (p≤0.01 for all) (table 2). Foot PN was present in 85.3% of the patients, with 80% having small fiber and 57% large fiber neuropathy; co-existing in 51.4% of the cases. PN was associated with age, smoking, foot ulceration, disease duration and corticosteroids use. 82% patients with PN reported minimum one neuropathic symptom, while 18% were asymptomatic. Patients with neuropathic symptoms reported worse physical function on the SSc Health Assessment Questionnaire (1.47 [IQR 0.95-1.89] vs 0.74 [IQR 0.46-1.38]; p=0.003), worse foot disability on the Manchester Foot Pain and Disability Index (median 22 [IQR 14-28] vs 18 [IQR 4-22]; p=0.01), and poorer QoL on the Systemic Sclerosis Quality of Life Questionnaire (21 [IQR 11-24] vs 12 [IQR 6-20]; p=0.009).
Conclusion: Foot PN is a common and disabling manifestation in SSc, involving small and large fibres. Small fibres are also present in the enteric nervous system, thus highlighting the potential for PN being a surrogate marker for GI autonomic neuropathy. These results show the importance of including PSN assessment as a part of the SSc workup.
dcSSc: diffuse cutaneous SSc; lcSSc: limited cutaneous SSc; mRSS: modified Rodnan skin score.
To cite this abstract in AMA style:
Alcacer-Pitarch B, di battista m, Redmond A, Keenan A, Di Donato S, Del Galdo F, Buch M. Prevalence and Impact of Peripheral Neuropathy in SSc: A Frequent and Disabling Manifestation in SSc, and a Potential Surrogate Marker for Autonomic Neuropathy [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-impact-of-peripheral-neuropathy-in-ssc-a-frequent-and-disabling-manifestation-in-ssc-and-a-potential-surrogate-marker-for-autonomic-neuropathy/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-impact-of-peripheral-neuropathy-in-ssc-a-frequent-and-disabling-manifestation-in-ssc-and-a-potential-surrogate-marker-for-autonomic-neuropathy/