Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis (PsA) can manifest with different musculoskeletal (MSK) features. Ultrasound (US) optimizes the assessment of the different MSK features in PsA. However, there is no consensus on which MSK sonographic lesions and what locations should be evaluated by US. The group for research and assessment of psoriasis and psoriatic arthritis (GRAPPA) have set a goal of defining the most prevalent locations for the various US lesions in order to reduce the number of scanned sites.
The aim of the study was to describe the prevalence and distribution of key sonographic MSK lesions in patients with PsA.
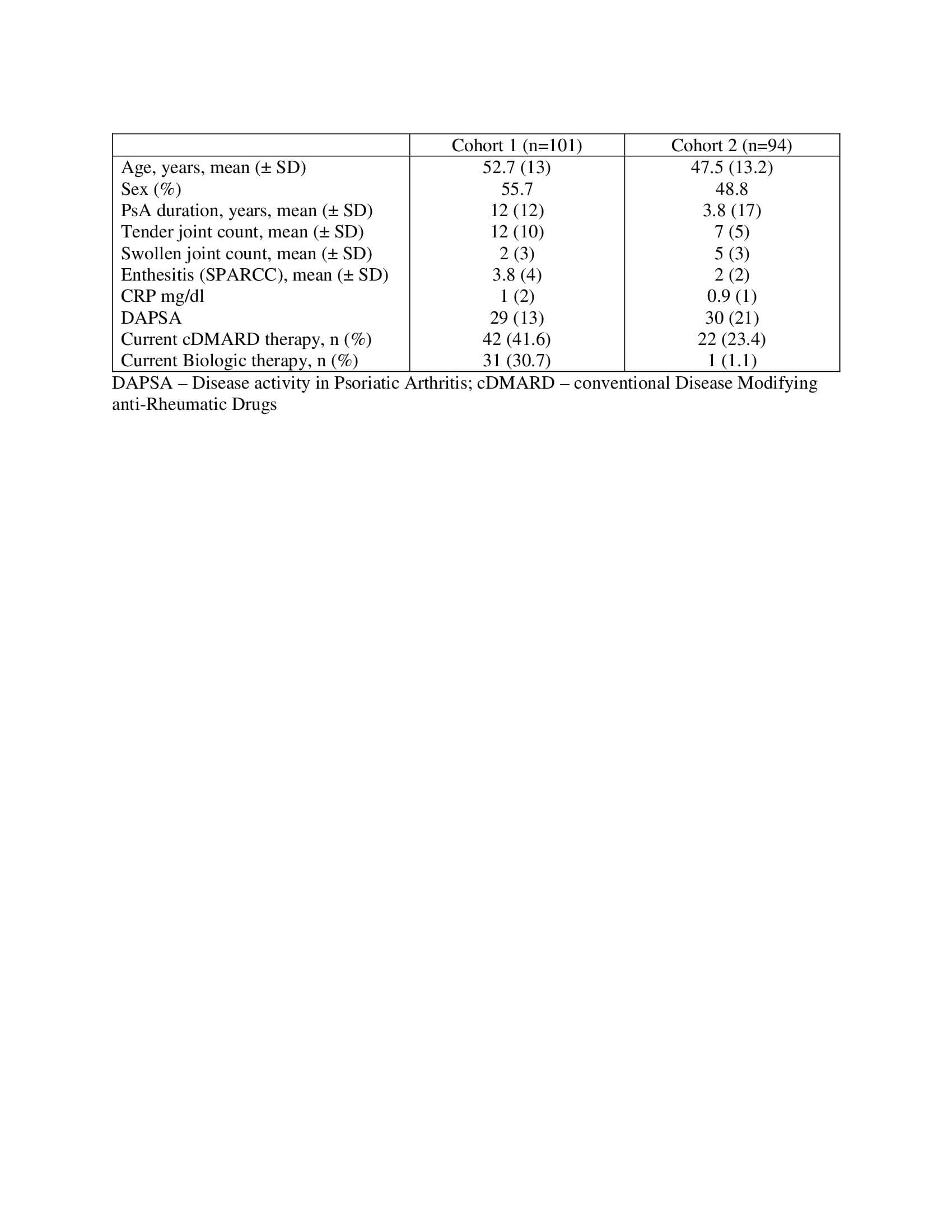
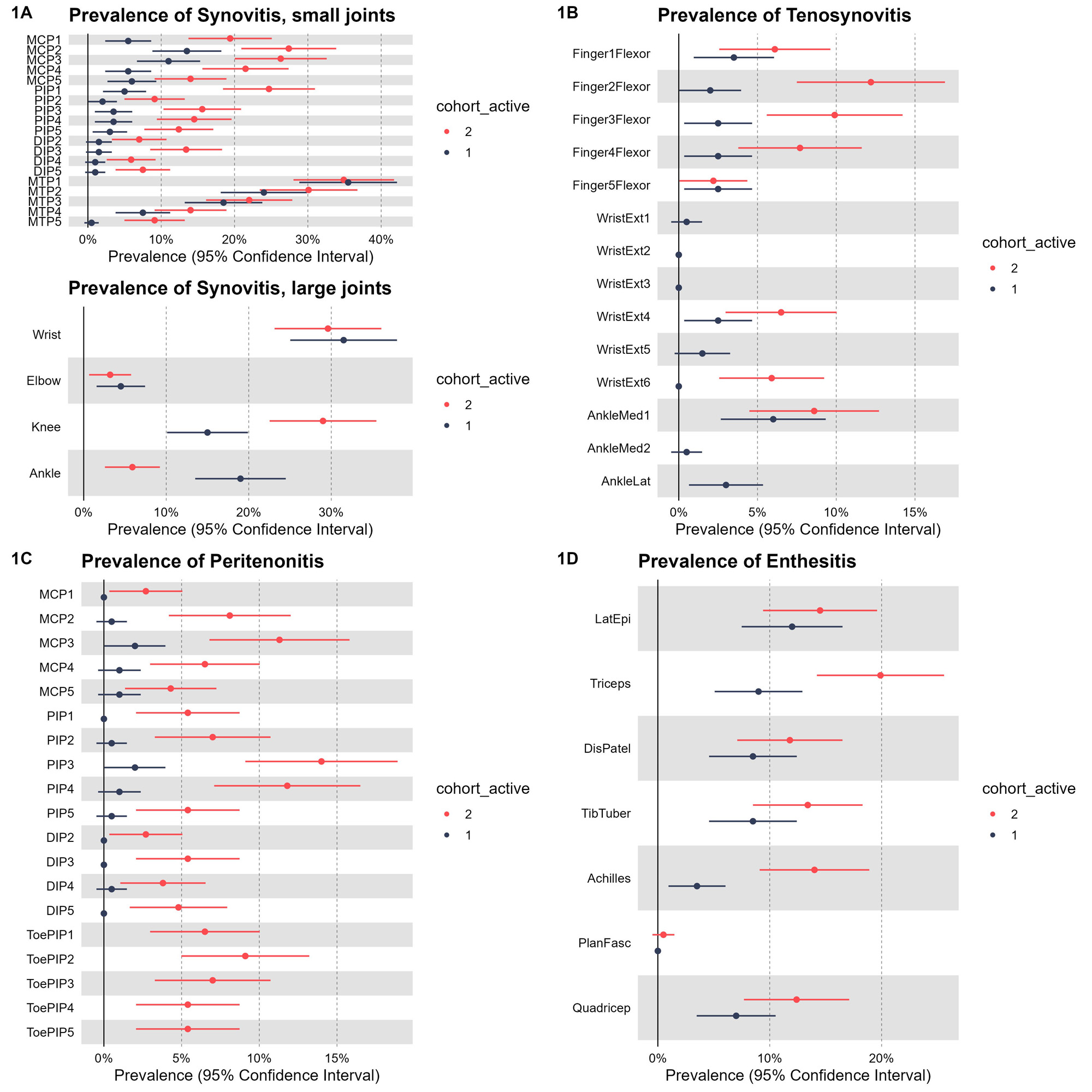
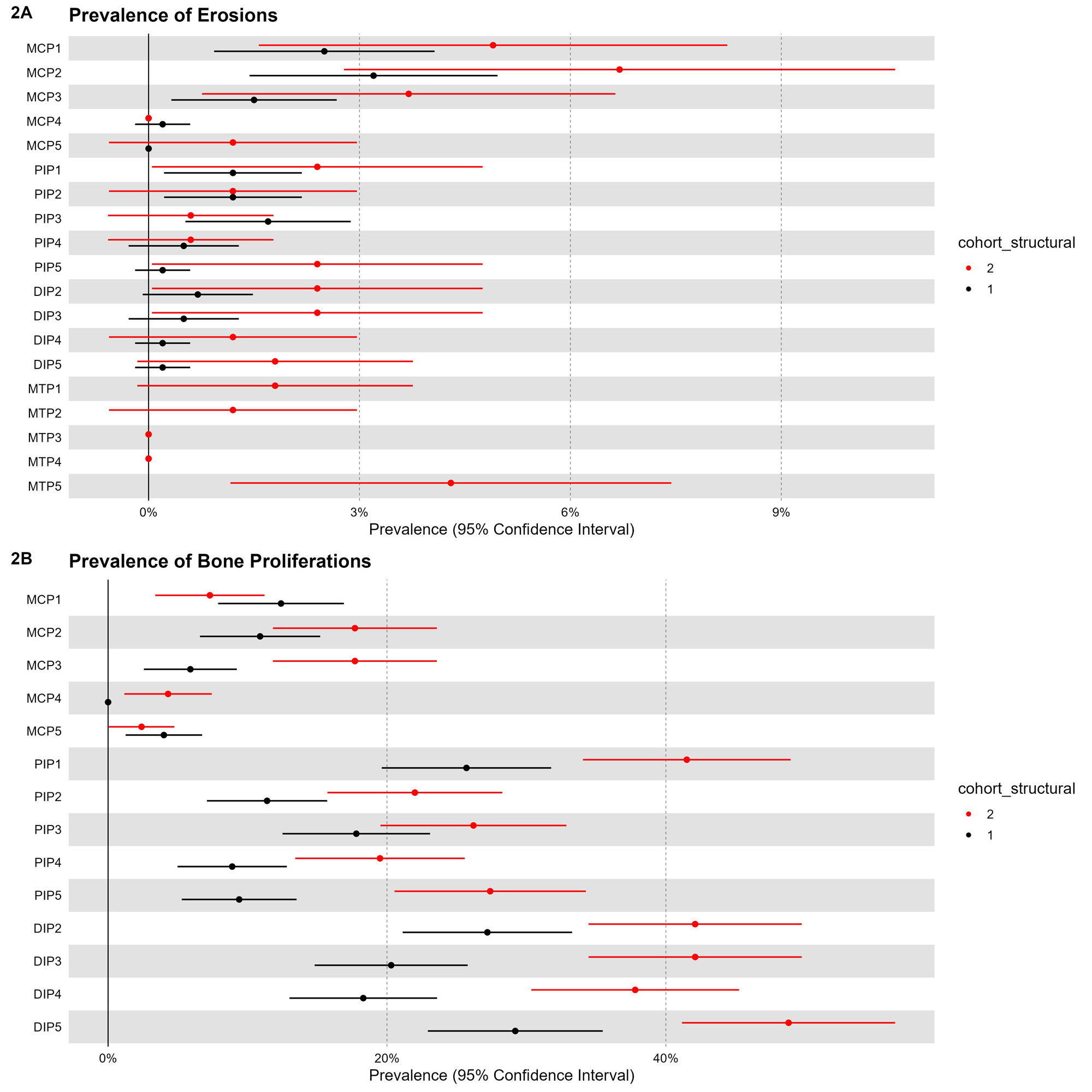
Methods: This study analyzed data from two prospectively recruited PsA cohorts. Cohort 1 included 101 patients with active PsA (DAPSA >14) and cohort 2 included 94 patients with active PsA prior to initiation of therapy. All underwent a comprehensive US assessment, including both gray scale (GS) and power Doppler (PD) of 50 joints, 40 tendons and 14 entheses. The following sonographic lesions were assessed by two sonographers blinded to clinical data: I. Inflammatory lesions – synovitis, tenosynovitis, peritenonitis and enthesitis and II. Structural lesions – periarticular erosions and bone proliferations. Presence or Absence of these lesions was determined based on previously suggested definitions by OMERACT (when available) or other publication and their prevalence by joint/tendon site was reported.
Results: In cohort 1, mean ± SD age was 52.7 ± 13 and 55.7% were females. In cohort 2, mean ± SD age was 47.5 ± 13.2 and 48.8% were females (Table 1). The most prevalent locations of the inflammatory lesions in both cohorts were (figure 1): Synovitis (small joints) – MCP2 (cohort 1: 13.5%, cohort 2: 27%), MCP 3 (cohort 1: 11%, cohort 2: 26%), IP1 (cohort 1: 5%, cohort 2: 24.5%) PIP 3 (cohort 1:3%, cohort 2: 16%), MTP 1 (cohort 1: 35.5%, cohort 2: 35%), MTP2 (cohort 1: 24%, cohort 2: 30%), MTP3 (cohort 1: 18.5%, cohort 2: 22%); Synovitis (medium-large joints) – wrist (cohort 1: 31.5%, cohort 2: 29%) and knee (cohort 1: 15%, cohort 2: 29%); Tenosynovitis – 2nd finger flexors (cohort 1: 2%, cohort 2: 8%) 3rd finger flexor (cohort 1: 2%, cohort 2: 6%), extensor digitorum (cohort 1: 2.5%, cohort 2: 6%), tibialis posterior (cohort 1: 6%, cohort 2: 8.5%); extensor peritenonitis –MCP3 (cohort 1: 2%, cohort 2: 12%), PIP 3 (cohort 1: 2%, cohort 2: 14%), PIP4 (cohort 1: 1%, cohort 2: 12%); Enthesitis – lateral epicondyle (cohort 1: 12%, cohort 2: 14%) and triceps (cohort 1: 9%, cohort 2: 20%). The most prevalent locations of the structural lesions (figure 2): Erosions – MCP1 (cohort 1: 4%, cohort 2: 4%), MCP2 (cohort 1: 6.5%, cohort 2: 6%), MCP3 (cohort 1: 3%, cohort 2: 3%), MTP5 (cohort 2: 4%); Bone proliferations – IP1 (cohort 1: 25%, cohort 2: 36%), DIP2 (cohort 1: 27.5%, cohort 2: 37%), DIP3 (cohort 1: 19.5%, cohort 2: 37%) and DIP5 (cohort 1: 28%, cohort 2: 44%).
Conclusion: This descriptive study provides comprehensive information on the most commonly affected sites for key inflammatory and structural domains in PsA. This information can inform efforts to develop reduced sonographic score to diagnose or monitor disease activity in PsA.
To cite this abstract in AMA style:
Polachek A, Furer V, Thib S, Mendel L, Elkayam O, Eder L. Prevalence and Distribution of Sonographic Elementary Lesions in PsA – Results of 2 Cohorts [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-distribution-of-sonographic-elementary-lesions-in-psa-results-of-2-cohorts/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-distribution-of-sonographic-elementary-lesions-in-psa-results-of-2-cohorts/