Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Literature describing the overlap syndrome of SSc and SLE is limited and has employed a range of case definitions. Our study sought to use the new EULAR/ACR SLE classification criteria to define and characterize SSc-SLE cases among our center’s SSc cohort.
Methods: A single-center, retrospective study of SSc patients was performed. A previously described cohort (Moore 2019) composed of African American and non-African American SSc patients matched 1:1 by sex, age, date of first visit, disease duration at first visit, and limited vs. diffuse cutaneous disease was used. The 2013 ACR/EULAR Classification Criteria for SSc were fulfilled in 91% of these patients. Patient data were re-abstracted to evaluate specifically for fulfillment of the 2019 EULAR/ACR Classification Criteria for SLE and the 2012 SLICC Criteria for the Classification of SLE. Demographic, laboratory, and clinical features and mortality were compared among SSc-SLE overlap and non-overlap SSc patients.
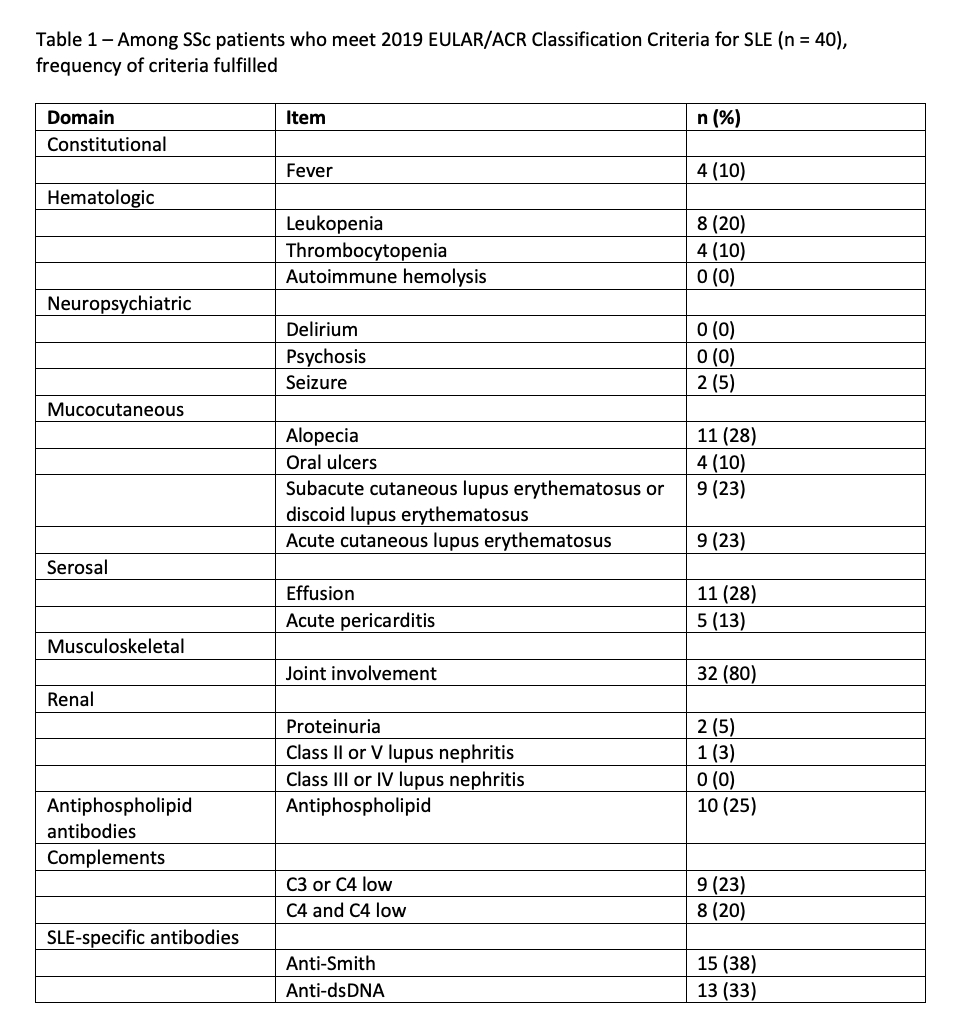
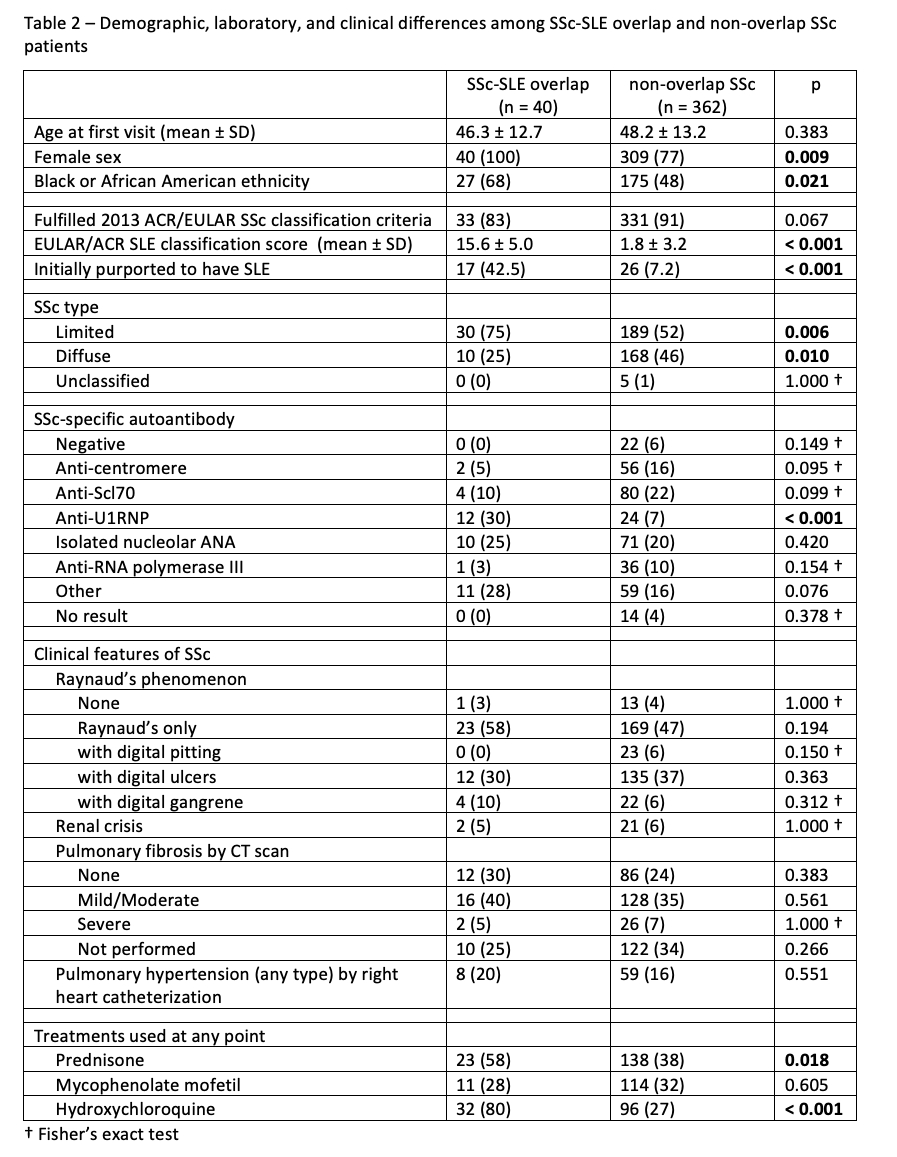
Results: 402 patients with SSc were analyzed. 40 (10%) of patients fulfilled the 2019 EULAR/ACR SLE criteria, 41 (10%) fulfilled the 2012 SLICC criteria, and 33 (8.2%) fulfilled both sets of criteria. Table 1 shows the frequencies of the criteria items among patients who fulfilled the EULAR/ACR criteria. Neuropsychiatric and renal involvement were rare. Table 2 compares the features of overlap and non-overlap SSc patients. An initial diagnosis of SLE was purported in 43% of the overlap patients and 7% of non-overlap patients (p < 0.001). Overlap patients were more likely to be female, be African American, and have limited cutaneous SSc. Anti-U1RNP antibody positivity prevalence was only 30% among overlap patients, and lower at 6.6% among non-overlap patients (p < 0.001). Overlap and non-overlap patients were similar in the prevalence of other SSc-specific autoantibodies, Raynaud’s phenomenon, scleroderma renal crisis, pulmonary fibrosis per CT scan, and pulmonary hypertension by right heart catheterization. Overlap patients were more likely to have received treatment with prednisone or hydroxychloroquine at any point. Death during follow-up occurred in 12 (30%) of SSc-SLE overlap patients and in 81 (22%) of non-overlap patients, but there was no difference in survival among the groups per log rank test (p = 0.404).
Conclusion: Approximately 10% of SSc patients fulfill the 2019 EULAR/ACR Classification Criteria for SLE. These SSc-SLE overlap patients comprise a distinct demographic, serologic, and clinical phenotype but sustain similar severe SSc-specific end-organ damage and mortality as non-overlap SSc patients. SLE patients with Raynaud’s should be evaluated for SSc-specific autoantibodies and clinical features.
To cite this abstract in AMA style:
Bass R, Moore D, Steen V. Prevalence and Characteristics of Systemic Sclerosis Patients Fulfilling the 2019 EULAR/ACR Classification Criteria for Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/prevalence-and-characteristics-of-systemic-sclerosis-patients-fulfilling-the-2019-eular-acr-classification-criteria-for-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-characteristics-of-systemic-sclerosis-patients-fulfilling-the-2019-eular-acr-classification-criteria-for-systemic-lupus-erythematosus/