Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial lung disease (ILD) is a rare and severe complication of systemic juvenile idiopathic arthritis (SJIA) that was recognized relatively recently, and its incidence appears to be rising. Much is still unknown about its optimal management.
Methods: With an institutional review board approval from Baylor College of Medicine, children under 16 years old with SJIA-associated lung disease (SJIA-LD) at Texas Children’s Hospital between 2014-2023 were identified. Demographics, clinical features, laboratory, radiographic findings, and therapies were collected and analyzed using standard descriptive statistics.
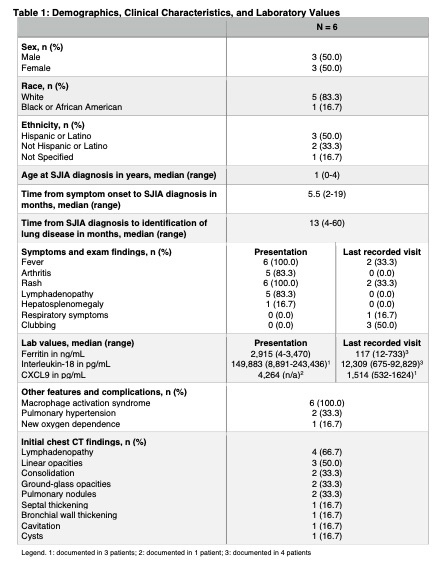
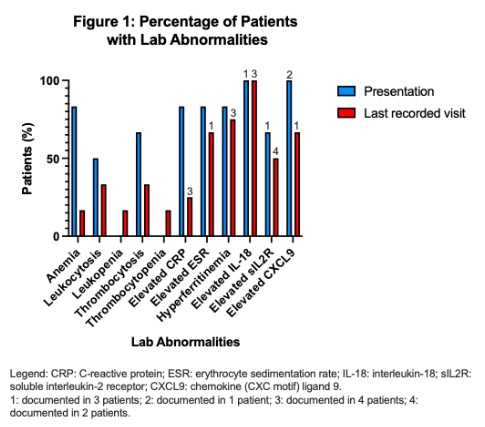
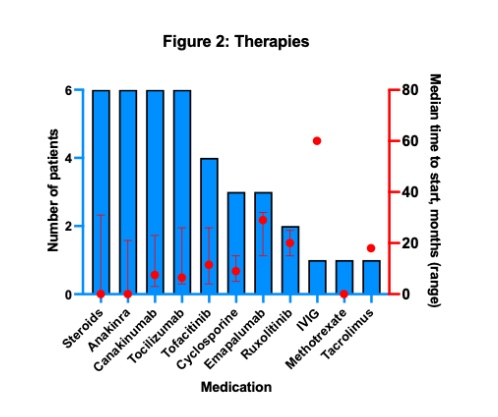
Results: Six children with SJIA-LD were identified. The median age in years at SJIA diagnosis was 1 (range 0-4), and patients were followed for a median of 30.5 months (range 15-82). There were equal numbers of males and females, most were white (83.3%, vs. 16.7% Black), and most were Hispanic (50.0%, vs. 33.3% not Hispanic and 16.7% not specified). Four patients (66.7%) had no significant medical history prior to SJIA presentation, while 1 patient had Trisomy 21, and another was a former 23-week preterm infant with associated complications, including bronchopulmonary dysplasia with tracheostomy dependence. All patients presented classically with fever, rash, and arthritis; none had respiratory symptoms or clubbing at SJIA diagnosis. The median time from SJIA diagnosis to identification of lung disease was 13 months (range 4-60). Imaging that led to the diagnosis was obtained due to respiratory symptoms in 3 patients (50.0%, of which one occurred in the setting of known rhinovirus) and for asymptomatic screening in 1case (16.7%). Two patients (33.3%) had incidental ILD on imaging obtained for other reasons. The most frequent pulmonary findings on the initial chest CT were linear opacities (50.0%), while 33.3% had ground-glass opacities. Two patients (33.3%) had pulmonary hypertension, and 1 (16.7%) developed a new oxygen dependence. In addition to corticosteroids, anti-IL1 and anti-IL6 drugs were the most utilized therapies. All patients had their disease course complicated by macrophage activation syndrome (MAS). The disease was difficult to control, and medication changes were common due to disease flares, challenges with the route of administration, infusion reactions, and side effects. At the most recent rheumatology visit, 5 patients (83.3%) were on dual biologic therapy, and 3 patients (50.0%) remained on chronic corticosteroids. No patients died during the study period.
Conclusion: All children in our SJIA-LD cohort were diagnosed with SJIA at an early age and had difficult-to-control disease, including elevated CXCL9 and IL-18 levels. Half of the patients had respiratory symptoms that led to chest imaging, while the other half had no respiratory symptoms. All experienced MAS and required aggressive therapy, often with dual biologics and chronic corticosteroids.
To cite this abstract in AMA style:
Altaffer A, Pereira M, De Guzman M, Ramirez A. Presentation, Management, and Outcomes of Systemic JIA-Associated Lung Disease: A Single Center Experience [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/presentation-management-and-outcomes-of-systemic-jia-associated-lung-disease-a-single-center-experience/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/presentation-management-and-outcomes-of-systemic-jia-associated-lung-disease-a-single-center-experience/