Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: To describe the clinical characteristics, therapies, and outcomes of patients with SLE and Posterior reversible encephalopathy syndrome (PRES).
Methods: We performed a multicenter cohort study in the United States from August 1999 – March 2021. We included patients with SLE who met the 2019 EULAR/ACR criteria and had incident PRES events. A case of incident PRES was defined as 1) the first acute neurological episode attributable to PRES, and 2) confirmation of vasogenic edema with MRI/CT and other causes excluded. A systematic literature review (SLR) was performed according to the PRISMA guidelines. We did a comprehensive search in multiple databases from their inception to October 20, 2021, in any language. Two reviewers independently screened and reviewed the articles and extracted information. We included case reports/case series reporting cases that met the inclusion criteria used for the cohort. We abstracted demographics, clinical and imaging features, treatment, and disease activity (SLEDAI). We summarized the days to recovery and length of stay (LOS). Neurological symptoms were classified as transient (≤3 days), persistent (≥14 days), or sequelae if permanent. The first available imaging was used to assess the distribution of vasogenic edema and other findings: restricted diffusion, hemorrhages, contrast enhancement, and angiography (MRI/CT). At least two consecutive imaging studies were required to determine the reversibility of edema. Patients were observed until death or last follow-up. The main outcomes after discharge were PRES relapses and all-cause mortality at 90 days. Cases in the cohort were combined with data from the SLR. Descriptive statistics were used to summarize pooled results.
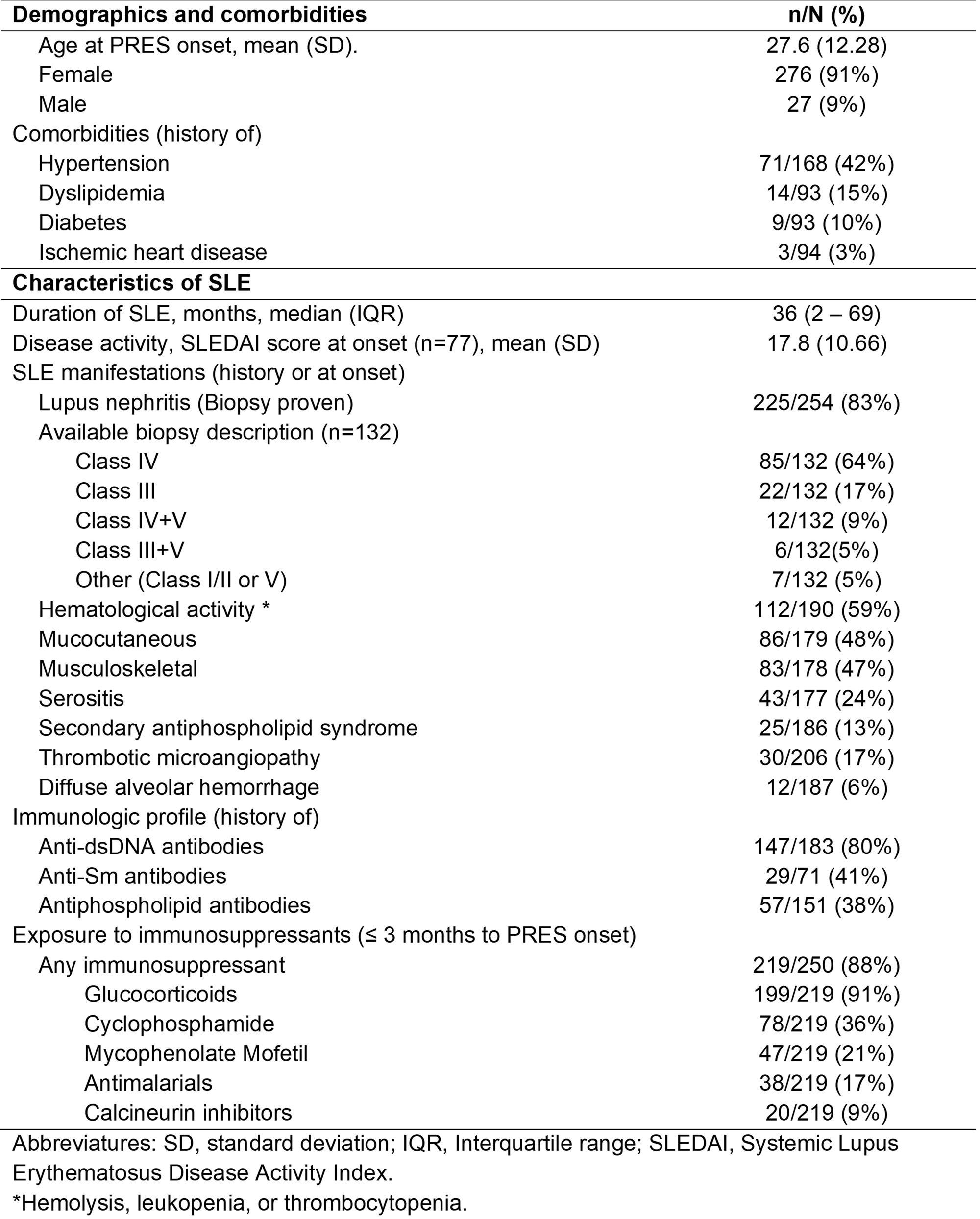
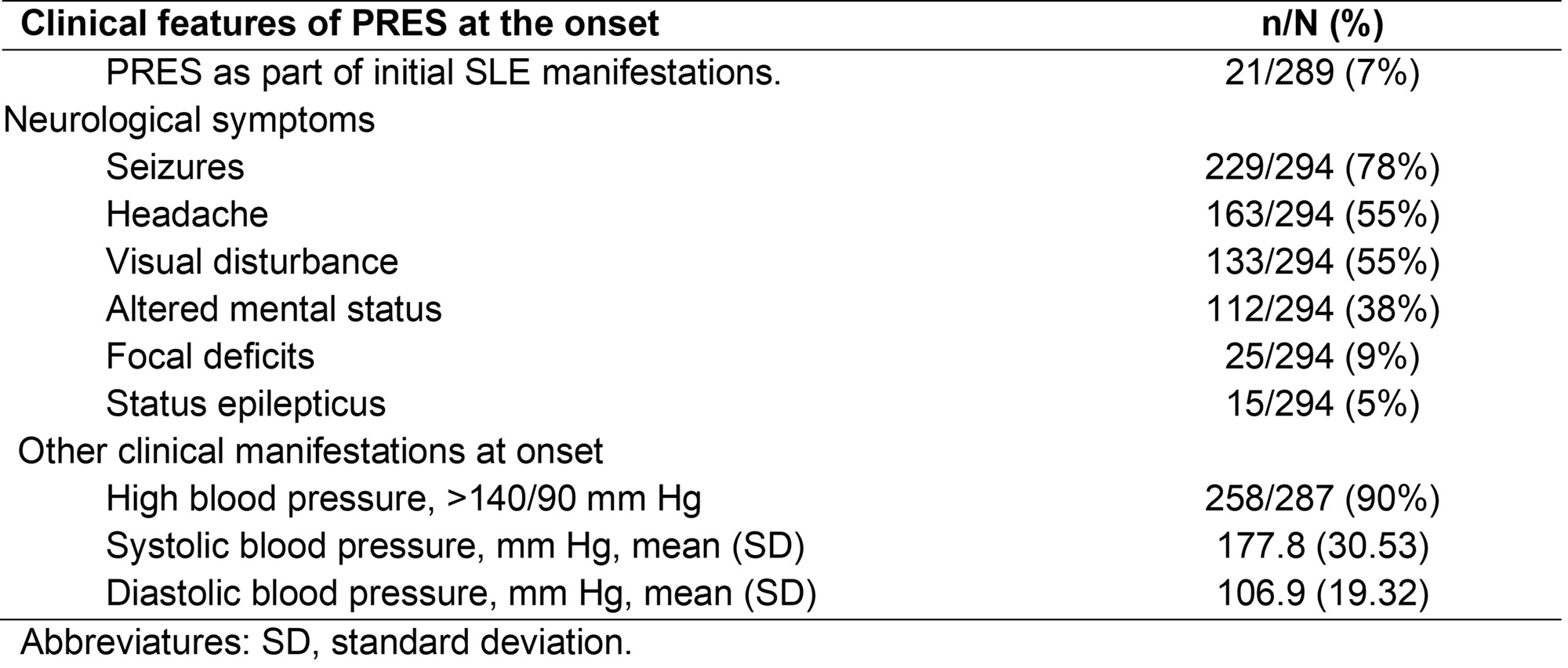
Results: A total of 303 cases were included, 50 (17%) from the cohort, and 253 (83%) from the SLR. The mean age at PRES onset was 27.6 years (SD 12.3), and 91% were women. Comorbidities included hypertension in 42%, dyslipidemia in 15%, and diabetes in 10%. The median (IQR) time between SLE and PRES was 36 months (2-92), and the median follow-up was one month (0.3-12). At onset, SLEDAI was 17.8 (SD 10.7), lupus nephritis was present in 83%, and the autoantibody profile consisted of Anti-dsDNA (80%), Anti-Sm (41%), and aPL (38%) (Table 1). Clinically, 90% had associated high blood pressure (BP) ( >140/90 mm Hg), and neurological manifestations were seizures in 78%, headache in 55%, visual disturbance in 45%, altered mental status in 38%, and focal deficits in 9% (Table 2). 97% of the patients survived and recovered after a median of 4 days (2-8), and LOS of 11 days (6-21). Among survivors, symptoms were transient in 45%, persistent in 19%, and 8% had sequelae. In the first imaging study, most had posterior and symmetric vasogenic edema. Among the 183 (60%) with follow-up imaging, brain edema improved in 97% after 15 days (7-49) (Table 3). Treatment strategies for PRES included BP control in 86%, antiepileptics in 64%, and new immunosuppressant therapy in 37%. After discharge, 12% relapsed after a median of 283 days (21-749). The 90-day mortality was 4%.
Conclusion: PRES in SLE develops predominantly in patients who have lupus nephritis. While most cases are reversible, sequelae are possible, and relapses are not uncommon.
To cite this abstract in AMA style:
Sanchez-Rodriguez A, Gonzalez-Treviño M, Langenfeld H, Crowson C, Valenzuela-Almada M, Rabinstein A, Prokop L, Valenzuela-Almada I, Duarte-Garcia A. Presentation and Outcomes of Posterior Reversible Encephalopathy Syndrome in Systemic Lupus Erythematosus: A Multicenter Cohort and a Systematic Literature Review [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/presentation-and-outcomes-of-posterior-reversible-encephalopathy-syndrome-in-systemic-lupus-erythematosus-a-multicenter-cohort-and-a-systematic-literature-review/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/presentation-and-outcomes-of-posterior-reversible-encephalopathy-syndrome-in-systemic-lupus-erythematosus-a-multicenter-cohort-and-a-systematic-literature-review/