Session Information
Date: Sunday, November 17, 2024
Title: SLE – Treatment Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Lupus nephritis is a well-known and severe complication in patients with systemic lupus erythematosus (SLE) that can lead to significant morbidity and mortality. Angiotensin-converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARBs) are known to decrease proteinuria, delay progression to end-stage renal disease (ESRD), and reduce SLE flares. Despite the clear benefits, studies indicate under-prescription and delayed prescription of these medications. Our goals for this preliminary study were to 1) identify which subspecialty groups (primary care, nephrology, and rheumatology) prescribe ACEi/ARBs in lupus nephritis patients, 2) evaluate prescription rates of ACEi/ARB in co-managed patients versus solo-managed patients, and 3) explore potential clinical and demographic factors influencing the decision to prescribe or not prescribe ACEi/ARBs to patients.
Methods: The patient cohort comprised patients greater than 18 years of age who were seen in an urban academic medical center from January 1, 2010, through September 12, 2020, with at least one ambulatory encounter and a diagnosis code associated with either lupus or lupus nephritis. Proteinuria was defined according to the American College of Rheumatology (ACR) definition of renal disease. Chronic Kidney Disease (CKD) was defined as GFR< 60. Hypertension was defined as having either a diagnosis code for hypertension, a blood pressure >140/90, or a prescription for an anti-hypertensive medication. Specialty visit type was identified by the specialty of providers associated with encounters. Clinical and demographic data were extracted from the electronic medical record. Data analysis was performed using a multivariate logistic regression.
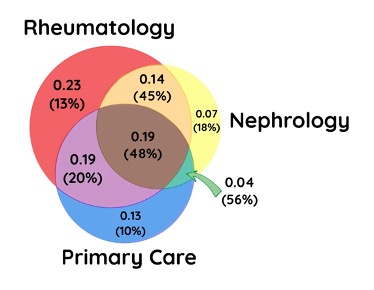
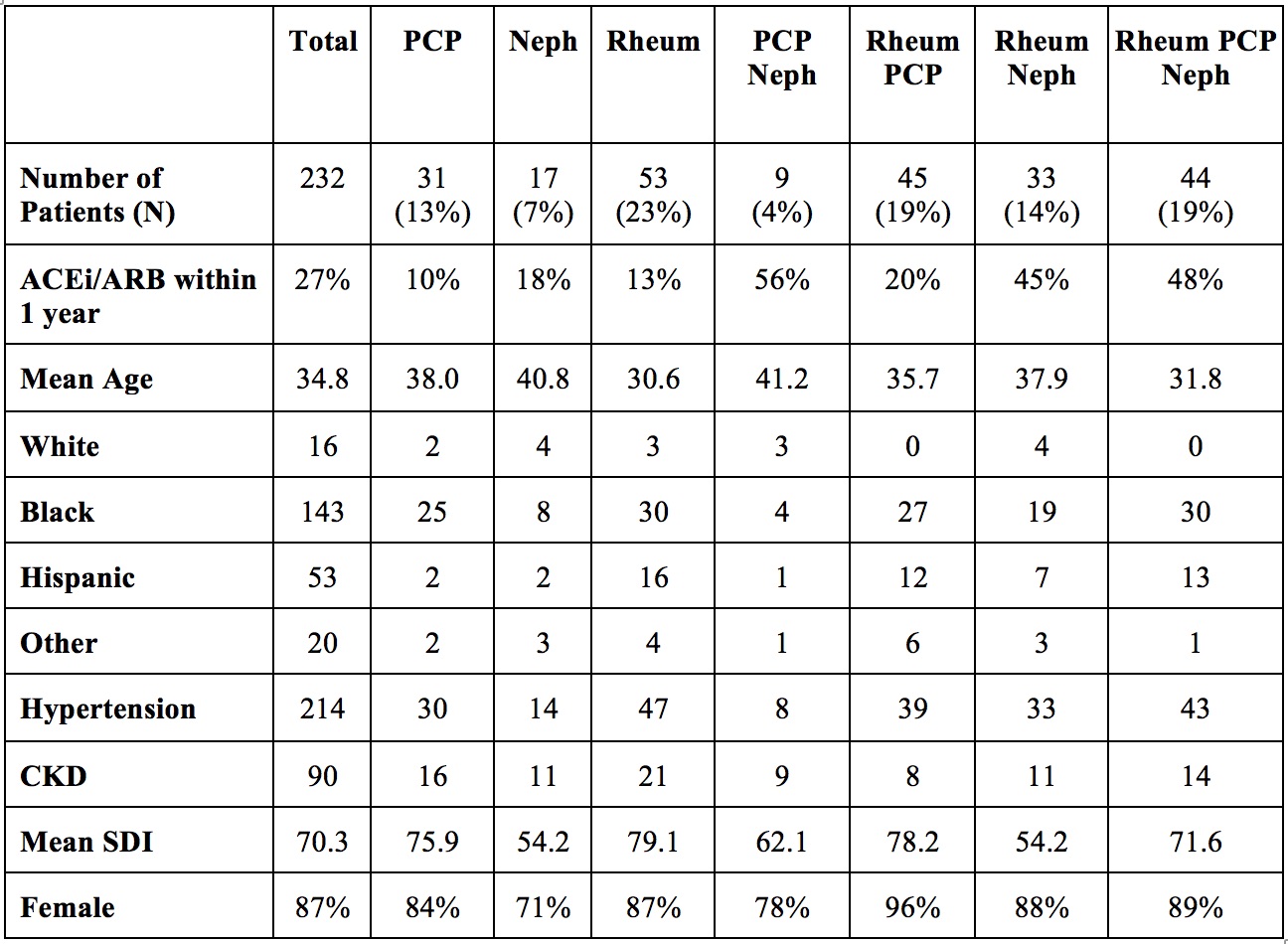
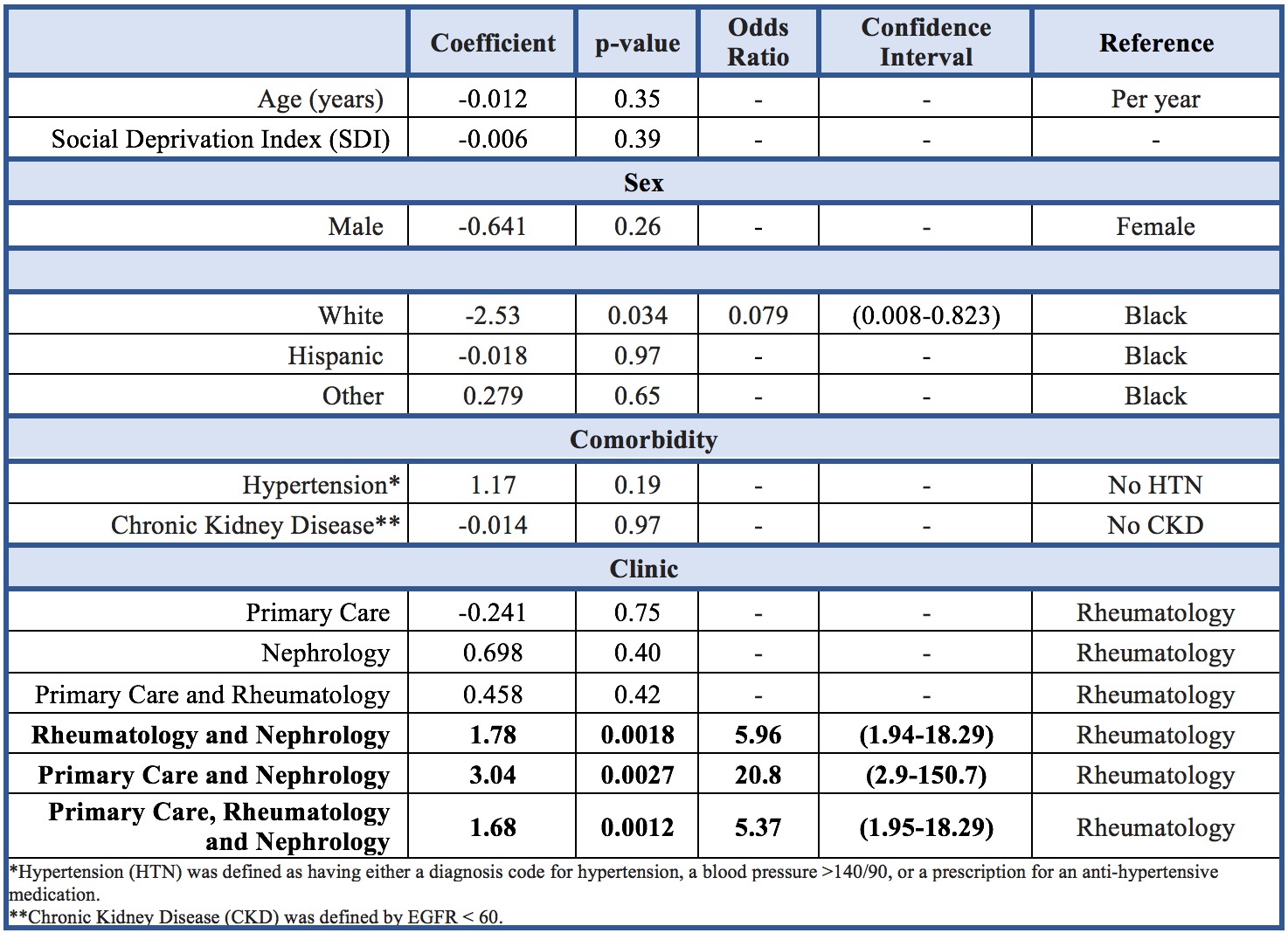
Results: A total of 232 patients were seen by primary care, rheumatology, nephrology, or a combination of these specialties. Patients co-managed with a nephrologist were more likely to be prescribed an ACEi/ARB than those seen by rheumatology alone. There was a trend toward a smaller proportion of Whites and males receiving an ACEi/ARB compared with Blacks and females, respectively. Age, Social Deprivation Index (SDI), and the presence of hypertension or chronic kidney disease did not affect ACEi/ARB prescription rates.
Conclusion: This study provides insight into the current prescribing practice of ACEi/ARBs for patients with lupus nephritis. Patients co-managed with a nephrologist were more likely to be prescribed an ACEi/ARB than those that were seen by rheumatology alone. Preliminary clinical and demographic data did not identify factors influencing the decision to initiate ACEi/ARB, but further study is needed. This information may help inform more targeted interventions to improve prescribing by specialty.
Rheumatology, Nephrology, and Primary Care are shown in red, yellow, and blue, respectively. The overlapping areas in the Venn diagram represent patients seen by multiple specialties. Decimals total 0.99 and represent the proportion of patients seen by each specialty or combination of specialties. The percentage in parenthesis is the percent of patients seen by that specialty or combination of specialties prescribed an ACEi/ARB.
PCP = Primary Care Physician; Rheum = Rheumatology; Neph = Nephrology
SDI = Social Deprivation Index; CKD = Chronic Kidney Disease defined as EGFR<60.
To cite this abstract in AMA style:
JANSZ J, Troy E, Galanter W, Adams E, Sweiss N, CHANG H. Prescription Rates of Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers in Lupus Nephritis: A Comparative Study Across Specialties [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prescription-rates-of-angiotensin-converting-enzyme-inhibitors-and-angiotensin-receptor-blockers-in-lupus-nephritis-a-comparative-study-across-specialties/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prescription-rates-of-angiotensin-converting-enzyme-inhibitors-and-angiotensin-receptor-blockers-in-lupus-nephritis-a-comparative-study-across-specialties/