Session Information
Date: Tuesday, November 10, 2015
Title: Reproductive Issues in Rheumatic Disorders: Basic and Clinical Aspects Poster Session
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
There is limited information regarding medication use patterns among pregnant
women with systemic lupus erythematosus (SLE). We
aimed to characterize trends of medications used to treat SLE before, during,
and after pregnancy, and to compare the use of other commonly used medications
among SLE pregnancies with non-SLE pregnancies.
Methods: Women with
pregnancies ending in live birth or stillbirth were identified from the Swedish
Medical Birth Register (MBR, 2006-2012). Prevalent
SLE during pregnancy was defined as 1) ³2 SLE ICD coded visits in inpatient or outpatient
care in the National Patient Register
(NPR) including ³1
SLE
code from a specialist and ³1 SLE
discharge before pregnancy or 2) ³1 SLE code from a specialist in the NPR and ³1 self-reported
diagnosis of SLE in the MBR. Women without SLE were sampled from the Total
Population Register. The Prescribed Drug
Register was used to identify prescription medications dispensed in the 3
months pre-pregnancy, during pregnancy, each trimester, the 3 months after
delivery (postpartum 1), and the 3-6 months after delivery (postpartum 2). No
information was available on intravenous infusions and medications obtained
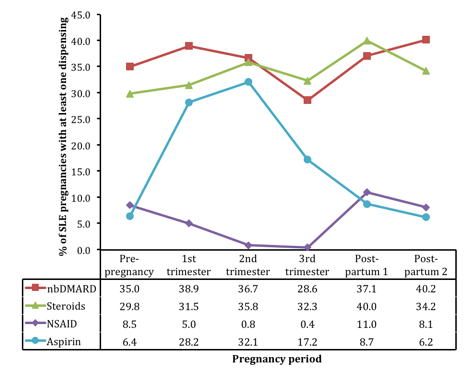
over-the-counter. We reported the prevalence of non-biologic disease modifying antirheumatic drugs (nbDMARDs), systemic
corticosteroids, and nonsteroidal anti-inflammatory
drugs (NSAIDs; aspirin reported separately) in SLE pregnancies by pregnancy
period. Then we calculated prevalence estimates of other medications (excluding
vitamins) that were dispensed during pregnancy to ³10% of women with SLE and for the same medications among non-SLE pregnancies.
Results:
We identified 483 pregnancies from 391 women with prevalent SLE and 5,723
pregnancies from 4,322 women without SLE. In SLE pregnancies, 49.3% had ³1
dispensing for nbDMARDs during pregnancy; the prevalence
was 48.0% for corticosteroids, 40.8% for aspirin, and 6.0% for other NSAIDs and
varied by period (Figure 1). Shorter exposure opportunity for preterm births
contributed to decreased prevalence in the 3rd trimester. The
prevalence of common medications among SLE pregnancies was 1.2 to 20-fold
higher than among non-SLE pregnancies: dalteparin
(20.9% vs 1.0%), paracetamol
(18.2% vs 2.9%), levothyroxine (15.9% vs 4.9%), phenoxymethylpenicillin
(14.3% vs 11.6%), pivmecillinam
(10.8% vs 4.7%), and omeprazole (10.4% vs 2.3%).
Conclusion:
In nearly half of SLE pregnancies from this population-based study, women were
dispensed nbDMARDs and corticosteroids. Other
commonly used medications among women with SLE had far higher prevalence
estimates versus the general population. Research regarding the benefits and risks
of these commonly used medications on SLE pregnancies, breast milk, and long-term
offspring outcomes is needed.
Figure.
Proportion of SLE pregnancies with ³1 dispensing for nbDMARDs, corticosteroids or NSAIDs by period.
To cite this abstract in AMA style:
Palmsten K, Simard JF, Chambers CD, Arkema EV. Prescription Medication Use in Sweden Among Pregnant Women with Systemic Lupus Erythematosus and General Population Comparators [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/prescription-medication-use-in-sweden-among-pregnant-women-with-systemic-lupus-erythematosus-and-general-population-comparators/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prescription-medication-use-in-sweden-among-pregnant-women-with-systemic-lupus-erythematosus-and-general-population-comparators/