Session Information
Date: Monday, November 14, 2022
Title: RA – Treatment Poster IV
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Use of prednisone in rheumatoid arthritis has been questioned because it may trigger side effects such as hyperglycemia and diabetes. However, disease activity (DAS) in RA has also been associated with glucose intolerance. Our objective is to assess whether in RA the use of glucocorticoids and the level of disease activity are associated with the development of hyperglycemia and diabetes.
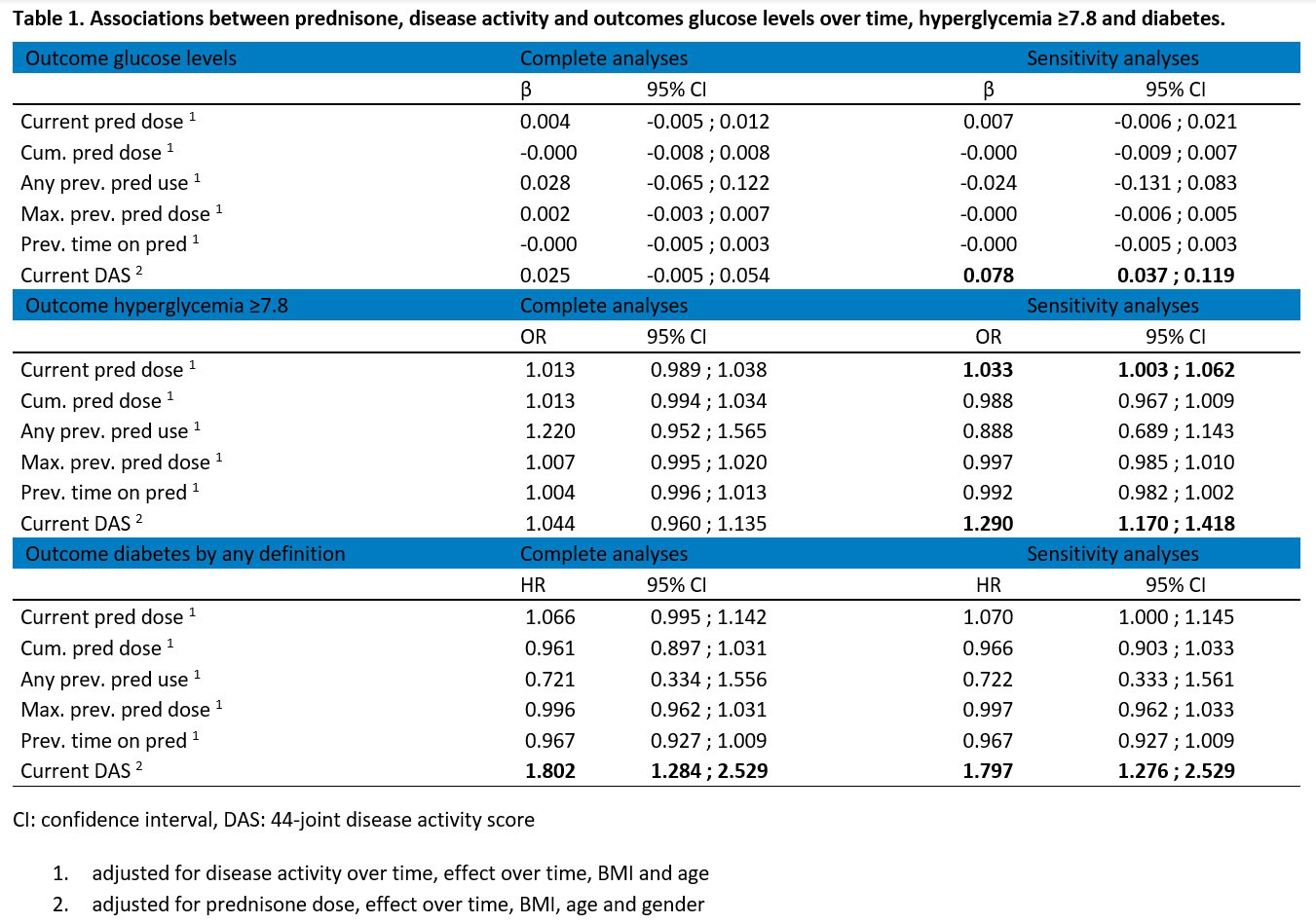
Methods: The BeSt study is a multicenter, assessor-blinded randomized controlled 10-years follow-up trial in 508 non-diabetic early RA patients. Patients were randomised to 4 dynamic DAS-steered DMARD treatment strategy groups. In all groups, prednisone was limited to 7.5mg/day by protocol, although preceded by a 7 week tapering schedule starting with 60mg/day in group 3. We performed a linear mixed model over time to assess whether DAS, prednisone dose or use was associated with glucose levels, a mixed effects logistic regression for the outcome hyperglycemia (glucose levels ≥7.8) and Cox regression analyses to investigate the relationship between DAS, prednisone dose or active use and development of diabetes (defined as either use of anti-diabetic medication or two instances of a glucose ≥ 11.1), assessed at 3-monthly visits. All analyses were adjusted for potential confounders (below table 1). Sensitivity analyses were performed in patients from the first instance of hyperglycemia, considered at high risk for diabetes and recurrence of hyperglycemia.
Results: 240 of 504 patients (48%) were treated with prednisone during the trial. Median (IQR) duration of prednisone use in these patients was 9 (6-15) months and cumulative doses ranged from 9900 to 28392 mg. The mean cumulative dose ranged from 352 mg in group 1 to 4878 mg in group 3. In total, 31/504 patients (6.2%) developed diabetes during the trial; 15 of these (48%) had been treated with prednisone (any dose).
In the main analysis in all patients, none of the ‘prednisone predictors’ were associated with our outcomes (table 1). In the sensitivity analyses after a first hyperglycemia, active prednisone dose only increased the odds of developing a recurrence of hyperglycemia (OR 1.033 per mg prednisone dose, 95% CI 1.003 ; 1.062). In the main analyses, disease activity was significantly associated with development of diabetes (HR 1.802, 95% CI 1.284 ; 2.529) but not with glucose values or hyperglycemia. In the sensitivity analyses, disease activity was associated with all outcomes.
Conclusion: In 504 early RA patients treated over 10 years to target DAS≤2.4, prednisone use and dose during treatment did not affect the risk of developing hyperglycemia or diabetes, but high disease activity did. Only in patients with a prior hyperglycemia did prednisone dose increase the odds of recurrence of hyperglycemia. This study suggests that the potential risks of prednisone use on development of hyperglycaemia and diabetes may have been mitigated by its effect on suppression of the disease activity.
To cite this abstract in AMA style:
Allaart C, Bergstra S, Huizinga T, van der Pol J. Prednisone Use and the Incidence of Hyperglycemia or Diabetes in Patients with Rheumatoid Arthritis; A 10-year Sub Analysis of the BeSt Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/prednisone-use-and-the-incidence-of-hyperglycemia-or-diabetes-in-patients-with-rheumatoid-arthritis-a-10-year-sub-analysis-of-the-best-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prednisone-use-and-the-incidence-of-hyperglycemia-or-diabetes-in-patients-with-rheumatoid-arthritis-a-10-year-sub-analysis-of-the-best-study/