Session Information
Date: Tuesday, November 19, 2024
Title: Abstracts: SLE – Diagnosis, Manifestations, & Outcomes III: Targets, Outcomes & Comorbidity
Session Type: Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Fractures are one of the most common damage items in the SLICC/ACR Damage Index. Although commonly attributed to corticosteroid use, the complexity of ways of examining steroid risk has not been studied before in a single cohort study. We examined both traditional risk factors and corticosteroid use in our analyses of risk factors for fracture.
Methods: We observed the rate of fractures in a large single-center SLE cohort from 1988 to 2023. A total of 2806 patients were included (92% female, 52% Caucasian, and 39% African American). Patients were observed for a total of 21,922 person-years (median duration of follow-up: 1.4 years, inter-quartile range: 1.4 to 11.8 years). Each month of follow-up was classified based on the patient’s demographics, clinical conditions, and treatments during that month. Fracture was defined, as per the SLICC/ACR Damage Index, as osteoporosis with fracture or vertebral collapse. Rates of fracture per person-year were calculated in subgroups. Estimates of rate ratios were based on pooled logistic regression models.
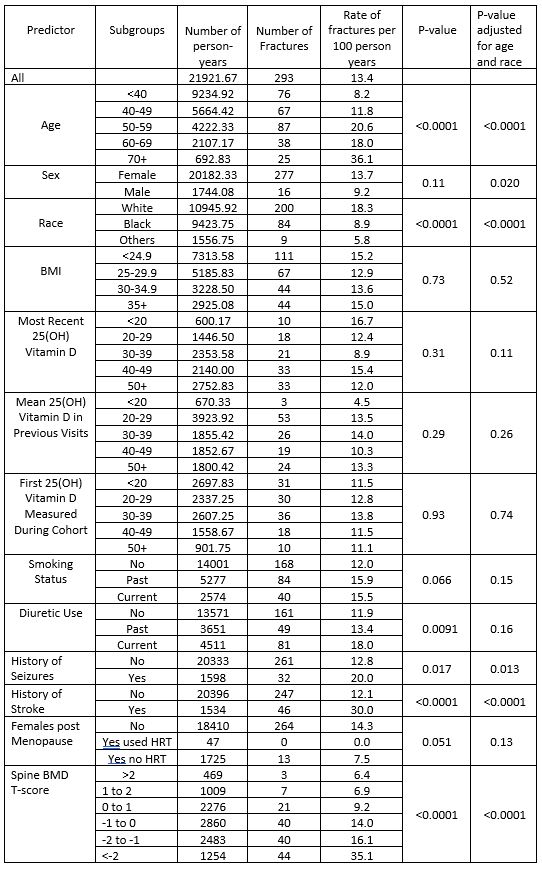
Results: We observed a total of 293 fractures for a rate of 0.13 per person-year. Table 1 shows the association of traditional non-SLE specific risk factors with fracture rates. Age, sex, race, history of stroke and low bone mineral density (BMD) were associated with risk of fracture. Sex, BMD, and stroke continued to be associated after adjustment for age and race. Low 25(OH) vitamin D blood level was NOT a risk factor.
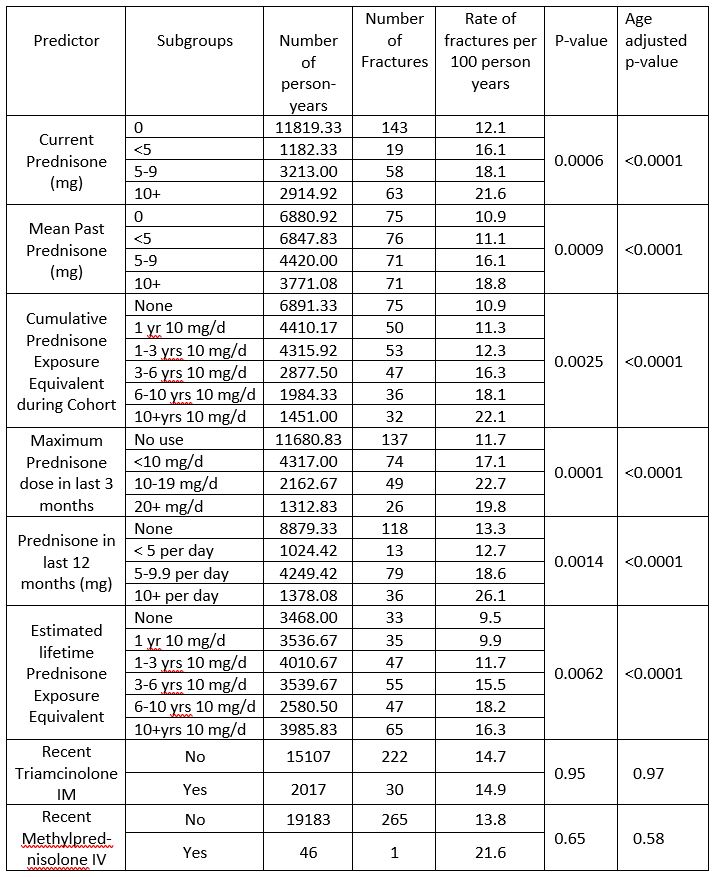
Table 2 examines the myriad ways that corticosteroids affect fracture risk in SLE. Neither intramuscular triamcinolone nor intravenous methylprednisolone (given at prior visit) increased fracture risk. However, ALL other ways of measuring steroid exposure (current, mean, cumulative, maximum, in last three months) increased fracture risk, including in age adjusted models.
Conclusion: Traditional risk factors (such as Caucasian race, female sex and low BMD) do increase fracture risk in SLE. Stroke – likely representing a risk of falls – is a significant risk factor, as well. Surprisingly, 25(OH) vitamin D level was NOT a risk factor. Prednisone use (but not intramuscular triamcinolone nor intravenous methylprednisolone) is the major risk factor, regardless of how it is measured. Our analyses confirm that even low dose prednisone (5-9.9 mg/day) significantly increases risk. Prednisone below 5 mg did also increase the risk. The EULAR 2023 guidelines highlight the need to avoid maintenance prednisone doses of over 5 mg/day. Our analyses confirm that this is a reasonable cut-off to reduce fracture, but would not prevent all fractures. Clearly, if corticosteroids are needed, intramuscular triamcinolone or intravenous methylprednisolone are preferable to oral corticosteroids.
To cite this abstract in AMA style:
Chao K, Fava A, Goldman D, Magder L, Petri M. Predictors of Fracture in SLE: A Longitudinal Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/predictors-of-fracture-in-sle-a-longitudinal-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-fracture-in-sle-a-longitudinal-cohort-study/