Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Rituximab (RTX) is widely used in immune mediated inflammatory disease (IMID) patients refractory to conventional treatment. Previous studies have indicated that RTX in IMID patients may lead to more severe COVID-19 disease outcomes. This study aims to characterize outcomes of hospitalized COVID-19 patients with IMIDs who received RTX treatment.
Methods: In this single center retrospective observational study, we included IMID patients with prior RTX use who got COVID-19 infection April 2021 to April 2023. COVID-19 was diagnosed by rRT-PCR assay detecting SARS-CoV-2 RNA. The demographics, serum markers, and medical outcomes were systematically reviewed from the electronic health records.
Average daily glucocorticoid dose (prednisone equivalent) per body weight (mg/kg/day) in the first 2 weeks after infection was adopted for analysis. We proposed the concept “very delayed viral shedding”, which referred specifically to a positive rRT-PCR result exceeding 28 days after diagnosis. COVID-19 disease severity was assessed per WHO classification. Outcomes included severe disease, very delayed viral shedding, and all-cause mortality (during hospitalization and in 6 months). For each outcome, we conducted univariate analysis and multivariate logistic regression. All analyses were conducted via R software.
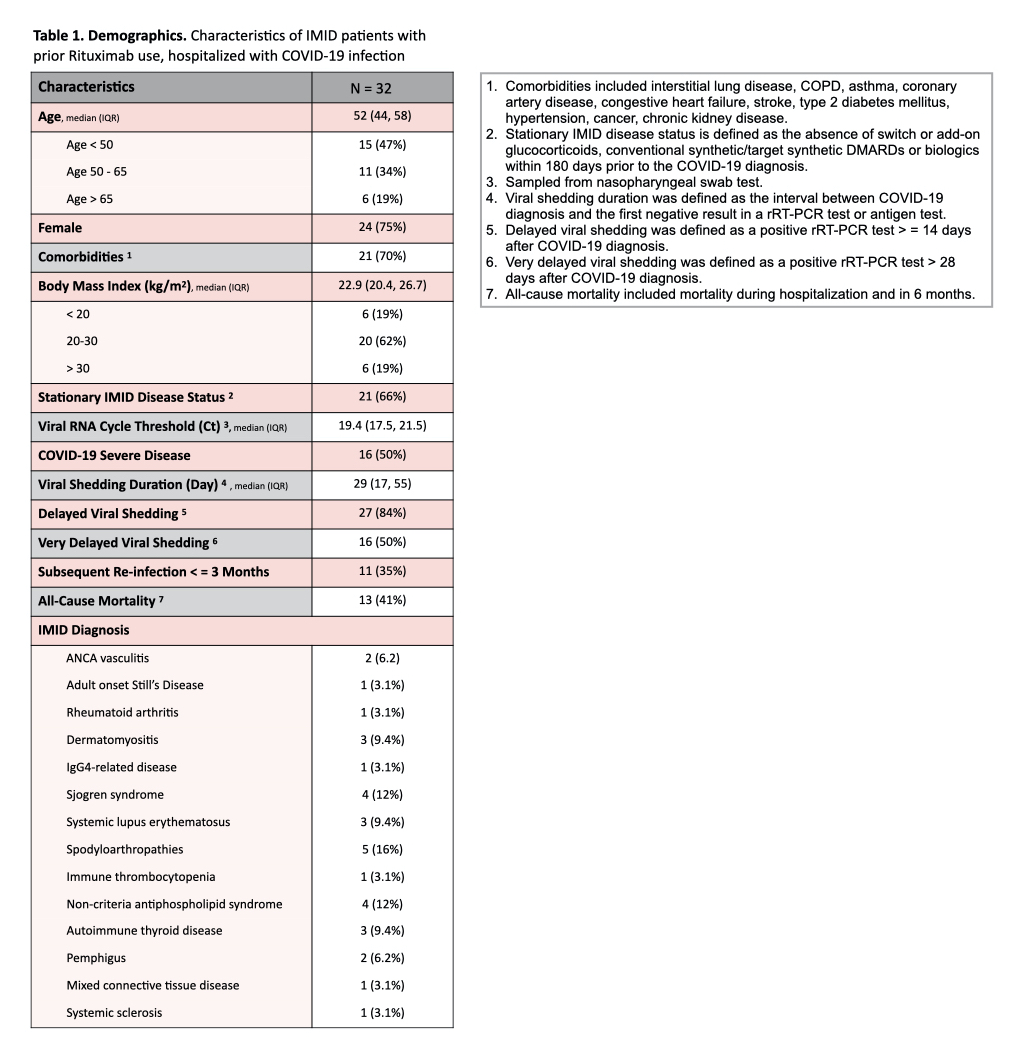
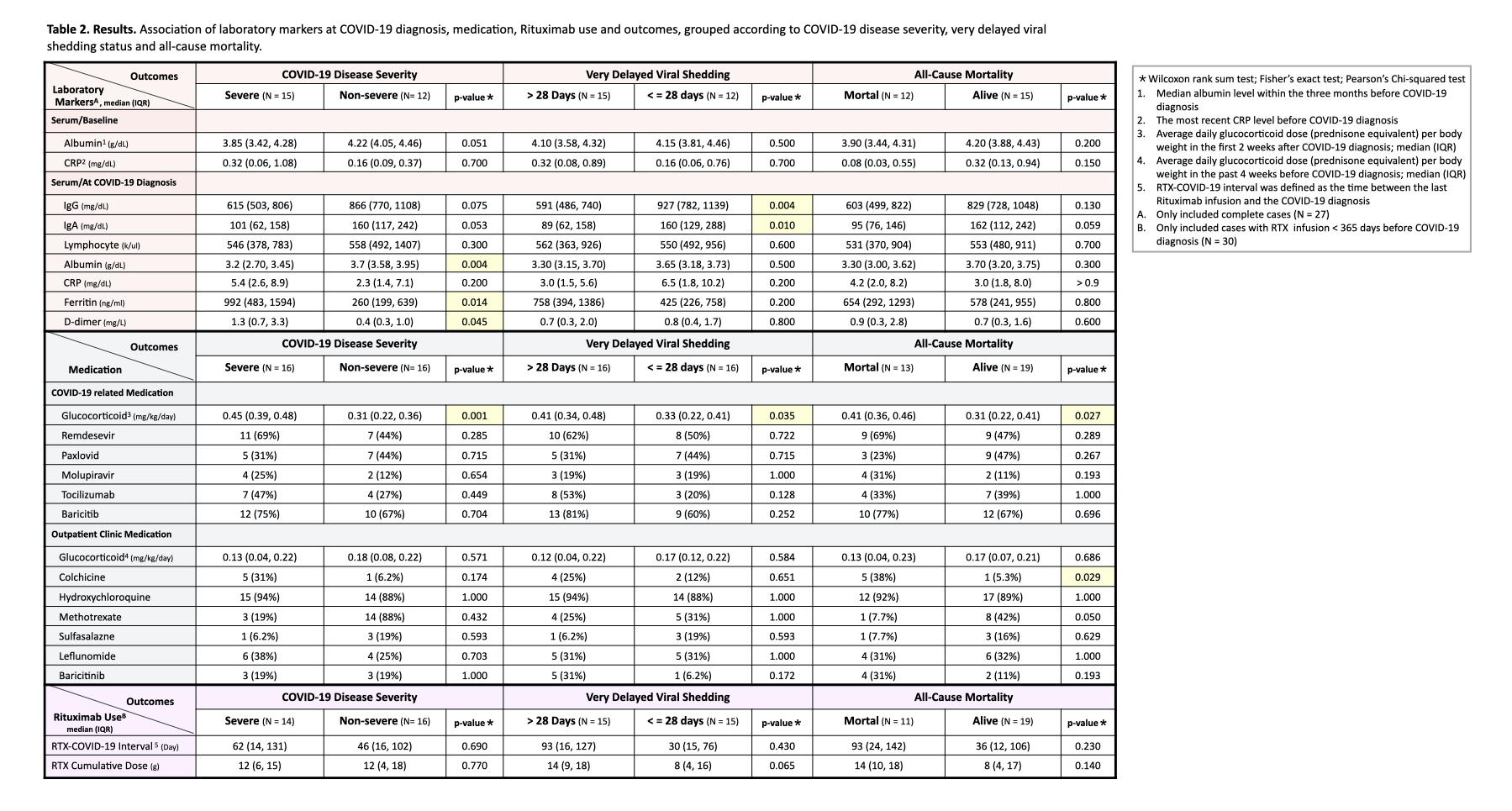
Results: A total of 32 IMID inpatients were included. Their characteristics are shown in Table 1. Sixteen (50.0%) had severe disease, 16 (50.0%) had very delayed viral shedding, and 40.6% died. Factors associated with outcomes are shown in Table 2. Lower baseline serum albumin (OR 0.100, 95% CI: -5.209 to -0.253), higher serum ferritin at diagnosis (OR 1.003, 95% CI: 5×10-4 to 0.006), and higher glucocorticoid dosage (OR 5.318, 95% CI: 0.798 to 2.544) were associated with severe COVID-19 disease. Lower serum IgG at diagnosis (OR 0.994, 95% CI: -0.012 to -0.002) and higher glucocorticoid dosage (OR 2.875, 95% CI: 0.102 to 2.010) were associated with very delayed viral shedding. Routine outpatient colchicine use (OR 16, 95% CI: 0.593 to 5.983) and higher glucocorticoid dosage (OR 3.170, 95% CI: 0.176 to 2.131) were associated with mortality.
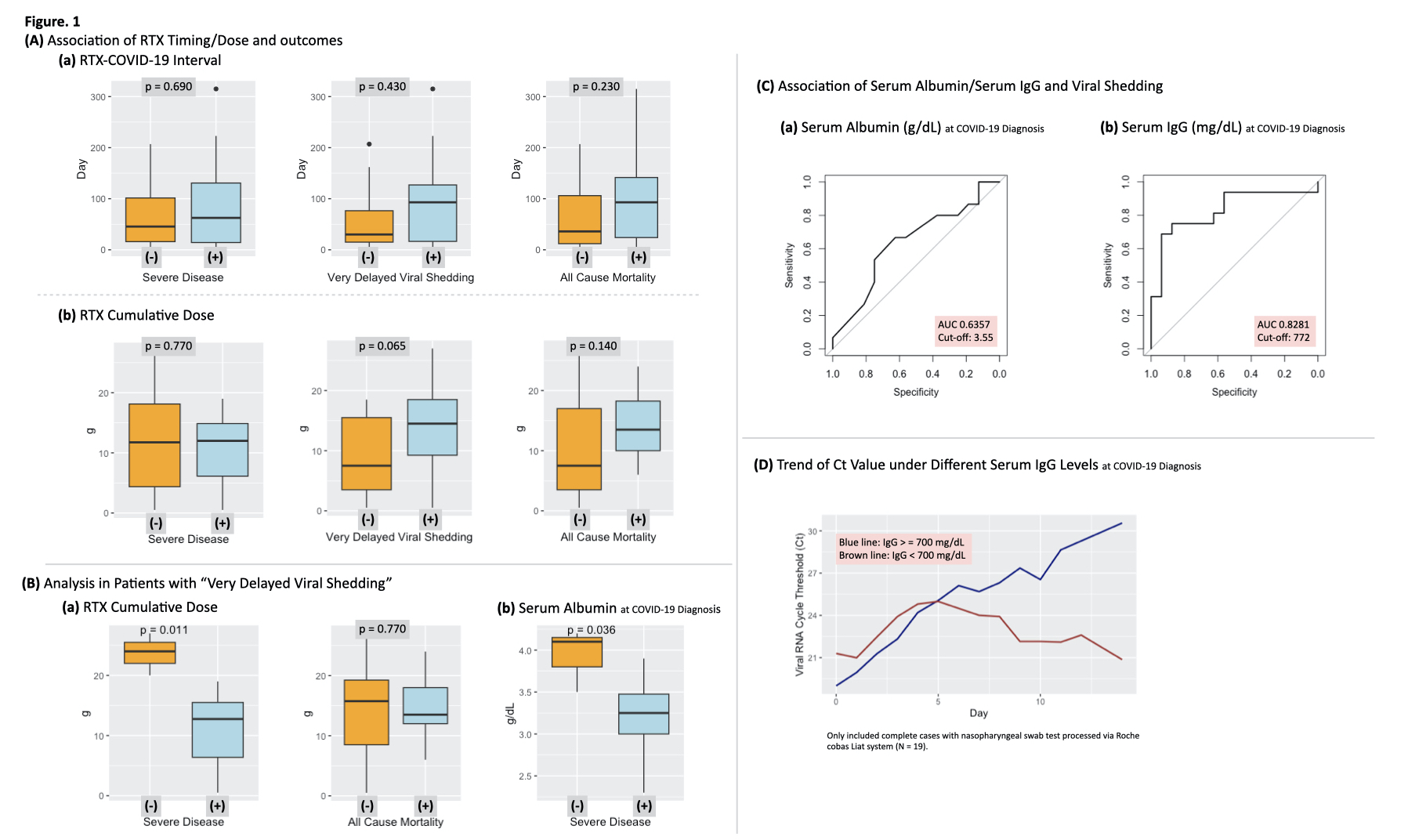
The time interval between the last RTX treatment and COVID-19 diagnosis, as well as the cumulative RTX dosage, were not associated with poor outcomes (Figure 1). However, higher cumulative dose tended to be associated with very delayed viral shedding. In patients with very delayed viral shedding, lower serum albumin levels at diagnosis, but not cumulative RTX dose, predicted severe disease. Although the viral cycle threshold (Ct) values increase during antiviral course, in the low serum IgG group, the Ct values wane as antiviral discontinued, potentially correlating with a subsequent poor prognosis (Figure 1D).
Conclusion: Lower serum albumin, higher serum ferritin and increased glucocorticoid dose, are indicative of severe inflammation. Our results suggest that severity of inflammation, rather than Rituximab dose or timing, is associated with poor outcomes. Future research should focus on determining the most optimal glucocorticoid dose for these patients, and whether extended antiviral treatment improves outcomes for those with low serum IgG.
To cite this abstract in AMA style:
Lai P, Chang T, Lan S, Cheng C, Lu C, Hsieh S. Predictors of Adverse Prognosis Following Hospitalization for COVID-19 Infection in Patients with Immune Mediated Inflammatory Diseases Treated with Rituximab [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/predictors-of-adverse-prognosis-following-hospitalization-for-covid-19-infection-in-patients-with-immune-mediated-inflammatory-diseases-treated-with-rituximab/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-adverse-prognosis-following-hospitalization-for-covid-19-infection-in-patients-with-immune-mediated-inflammatory-diseases-treated-with-rituximab/