Session Information
Date: Friday, March 31, 2023
Title: Poster Breakout 6 - Systemic JIA: Genomics, Transcriptomics & Disease States
Session Type: Breakout Session
Session Time: 4:30PM-5:00PM
Background/Purpose: Systemic juvenile idiopathic arthritis (sJIA) is a rare autoinflammatory disease of unknown etiology. Several uncontrolled studies showed that early treatment with anakinra is associated with a better outcome, according to the “window of opportunity” hypothesis. However, little evidence is available on withdrawal strategy. Anakinra withdrawal modalities are still heterogeneous among the different rheumatology centres. The aim of this study was to describe our strategy for anakinra withdrawal in sJIA patients following achievement of clinical inactive disease (CID) and to evaluate the association between clinical variables at baseline, including disease duration, and persistence of remission.
Methods: We retrospectively analysed data of 39 sJIA patients followed in our centre who withdrew anakinra after reaching CID off glucocorticoids for at least 6 months before withdrawal. Eight patients withdrew anakinra abruptly while 31 patients did it after tapering throughout one or two steps (alternate-day and/or once every three days regimens) of anakinra administration. All patients underwent a 24 months follow up after withdrawal. They were subsequently divided into two groups according to presence or absence of disease flare during the follow up. Demographic, clinical and laboratory data were evaluated in univariate and multivariate analysis as predictors of flare.
Results: During the follow up, 10/39 patients (25.6%) flared after a median time from anakinra withdrawal of 7.9 months. In univariate analysis the variable most strongly related with the absence of flare was the disease duration from the onset anakinra initiation (p = 0.0046), with an optimal cut-off of 3 months. Patients who started anakinra ≥ 3 months after disease onset had an 8-fold higher risk of flare after anakinra discontinuation (CI 95 2.0-32.4; p = 0.0003) (Figure 1). Furthermore, we observed that a higher dose of anakinra (³ 2 mg/kg/day) was associated with a lower risk of flare (p = 0.065). We also demonstrated that patients who tapered therapy before withdrawal were significantly associated with a lower percentage of flare compared to the ones who withdrew anakinra abruptly, with a 4-fold lower risk of flare (CI 95 1.47-10.1; p = 0.0164). In a model analysing at the same time disease duration, anakinra dose at baseline and anakinra tapering, disease duration ≥ 3 months at baseline resulted to be the only variable significantly associated with flare after anakinra withdrawal with an Odds Ratio of 15.16 (CI 95 1.7-131.9; p = 0.014).
Conclusion: Our results strengthen the evidence on IL-1 inhibition in sJIA treatment and provide new ones supporting the “window of opportunity” hypothesis. Early anakinra treatment may predict a good short-term outcome and also potentially prevent the development of a persistent disease course. These observations have a strong clinical relevance, an early diagnosis and a targeted treatment could control the disease and could also modify its natural history.
References:
- Nigrovic PA. Review. Arthritis Rheumatol 2014; 66:1405-13.
- Pardeo M, et al. Arthritis Rheumatol 2021; 73:1053-1061.
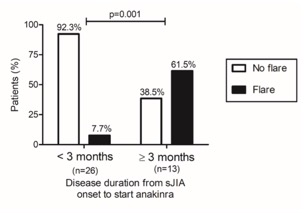 Figure 1. Relationship between disease duration from disease onset to anakinra initiation and rate of flare within the 24 months follow up after anakinra withdrawal.
Figure 1. Relationship between disease duration from disease onset to anakinra initiation and rate of flare within the 24 months follow up after anakinra withdrawal.
To cite this abstract in AMA style:
Nardini G, Bracaglia C, Pires Marafon D, Sacco E, De Matteis A, Caiello I, Prencipe G, De Benedetti F, Pardeo M. Predictive Factors of Long-lasting Remission Following Anakinra Withdrawal in Patients with Systemic Juvenile Idiopathic Arthritis After Achievement of Clinical Inactive Disease [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/predictive-factors-of-long-lasting-remission-following-anakinra-withdrawal-in-patients-with-systemic-juvenile-idiopathic-arthritis-after-achievement-of-clinical-inactive-disease/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictive-factors-of-long-lasting-remission-following-anakinra-withdrawal-in-patients-with-systemic-juvenile-idiopathic-arthritis-after-achievement-of-clinical-inactive-disease/
