Session Information
Date: Tuesday, November 9, 2021
Title: Pediatric Rheumatology – Clinical Poster III: Miscellaneous Rheumatic Disease (1614–1644)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Uveitis is the main extraarticular complication of juvenile idiopathic arthritis (JIA) with still a significant impact on JIA morbidity, despite continuous improvement in systemic treatment. Although antinuclear antibody positivity and early onset of JIA have been associated with a high risk of uveitis onset, no clinical features have been widely recognized as predictive factors for JIA-associated uveitis (JIA-U) lack of response to treatment, so far. The aim of our study is to investigate clinical features associated with lack of response to systemic treatment in a long-term cohort of patients with JIA-U.
Methods: Clinical records of patients with JIA-U were retrospectively reviewed with regard to clinical features, therapeutic choices and outcome. The role of potential predictors for lack of response to treatment has been assessed at bivariate and multivariate levels. Furthermore, a multivariable logistic model has been applied in order to estimate the strength of association between predictors and outcome, adjusting for potential confounders.
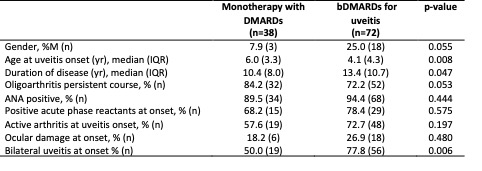
Results: Data from 152 JIA-U patients were analysed (82.2% female), with a median follow up of 12.0 years (IQR 9.9) and a median age at uveitis onset of 4.8 (4.1) years. In 72 patients (43.4%) at least one biologic DMARD (bDMARDs) to control uveitis was required. Compared to patients responsive to a monotherapy with a DMARD (n=38), children requiring a bDMARDs for uveitis had a lower median age at uveitis onset, a longer disease duration and a greater frequency of bilateral uveitis at onset (Table 1). No difference was observed in uveitis activity grade at onset. Despite similar frequency of ocular damage at onset, patients not responsive to DMARDs showed a higher percentage of ocular damage at last visit (66.7% vs 39.5% p=0.011). Multivariable analysis confirmed younger age at disease onset as an independent factor for lack of response to DMARDs (p 0.018). Male gender is associated with higher frequency of ocular surgery (33.3% vs 12.4%, p=0.043), and, despite the inaccuracy of the estimate due to limited sample size, acts as an independent factor in multivariable analysis with an almost 9 times higher risk to lack of response to DMARDs (p=0.049).
Conclusion: Younger age at uveitis onset and male gender are predictors of a worse response to DMARDs, while the length of follow-up exerts a confounding effect on bilateral uveitis. Children resistant to conventional treatment need prompt recognition and additional strategies to improve long-term outcome.
To cite this abstract in AMA style:
Minoia F, Marelli L, Pregnolato F, Beretta G, Mapelli C, Leone G, Cincinelli G, Nucci P, Giani T, Miserocchi E, Cimaz R. Predictive Factors for Lack of Response to Treatment in a Long-term Cohort of Patients with Juvenile Idiopathic Arthritis-associated Uveitis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/predictive-factors-for-lack-of-response-to-treatment-in-a-long-term-cohort-of-patients-with-juvenile-idiopathic-arthritis-associated-uveitis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictive-factors-for-lack-of-response-to-treatment-in-a-long-term-cohort-of-patients-with-juvenile-idiopathic-arthritis-associated-uveitis/