Session Information
Date: Sunday, November 5, 2017
Title: Systemic Sclerosis, Fibrosing Syndromes and Raynaud's – Clinical Aspects and Therapeutics Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
No data are available to distinguish between progressive and stable patients when mild lung fibrosis is diagnosed in systemic sclerosis (SSc) patients. This study aimed to identify clinical and laboratory parameters that can predict the progression of interstitial lung disease (ILD) within 1 year in patients with mild SSc-ILD.
Methods:
Data prospectively collected in our local SSc cohort were analyzed in this observational study. Inclusion criteria were: diagnosis of SSc fulfilling ACR/EULAR 2013 criteria, diagnosis of ILD by HRCT, < 20% lung involvement extent on HRCT at the first visit (baseline), available HRCT and pulmonary function tests at baseline and annual follow-up visits (12±3 months), no concomitant with PAH.
The primary endpoint, progression of ILD was defined if any of the following parameters was fulfilled : > 20% extent of lung involvement on HRCT at any follow-up visit, decrease in FVC ≥15% within 1 year, or decrease in FVC ≥ 10% and DLCO ≥ 15% within 1 year.
Candidate predictors for logistic regression were selected by expert opinion based on clinical consideration. Receiver Operating Characteristic (ROC) curve analysis was performed to determine the optimal cut-off value for each significant continuous parameter.
Results:
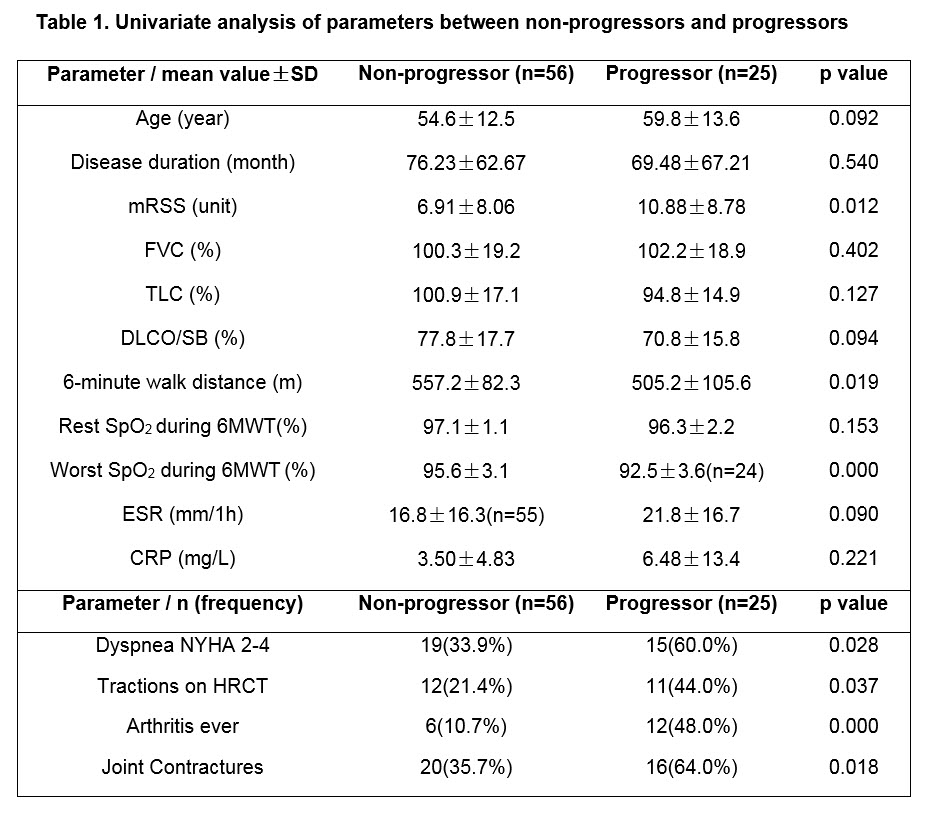
From the 81 patients included, 25 (30.9%) had progression of ILD. Differences of parameters between progressors and non-progressors were analyzed by univariate analysis (Table 1).
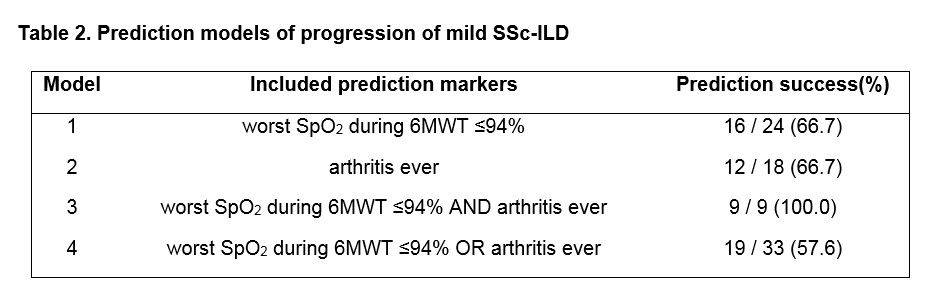
Three candidate predictors reflecting the overall disease severity including worst SpO2 during 6-minute walk test (6MWT), arthritis ever and modified Rodnan skin score (mRSS) were selected for logistic regression by expert opinion. The final regression model identified worst SpO2 (p=0.011, OR: 0.78, 95% CI 0.64 to 0.94) and arthritis ever (p=0.002, OR: 7.15, 95% CI 2.01 to 25.48) as independent predictors. The ROC curve analysis identified the best cut-off value for worst SpO2 as 94% (area under the curve: 0.78, sensitivity 0.667, specificity 0.857).
By employing combination of both predictors, the prediction model increased the prediction success rate from 30.9% in the whole cohort to 100% in the optimized enrichment cohort (Table 2).
Conclusion:
Our study identified exercise-induced SpO2 decline and arthritis ever as independent predictor of progression of mild SSc-ILD within 1 year. The derived evidence-based prediction model might be helpful for the risk stratification of this subgroup in clinical practice and cohort enrichment for future clinical trial design.
To cite this abstract in AMA style:
Wu W, Jordan S, Becker MO, Dobrota R, Ye S, Maurer B, Distler O. Prediction of Progression of Interstitial Lung Disease in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/prediction-of-progression-of-interstitial-lung-disease-in-patients-with-systemic-sclerosis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prediction-of-progression-of-interstitial-lung-disease-in-patients-with-systemic-sclerosis/