Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Antiphospholipid syndrome (APS) is a significant cause of morbidity and mortality in patients with SLE and lupus anticoagulant (LAC) positivity is the best predictor of thrombosis. However, in SLE LAC positivity can fluctuate over time. We determined the probabilities of transitions between the lupus anticoagulant states and thrombosis, and identify predictors of these transitions.
Methods: SLE patients in a longitudinal cohort had LAC determined using ISTH guidelines at every visit. A dRVVT of 45 or more seconds and a positive confirm ratio of more than 1.4 were defined as positive for LAC. Missing values were handled using multiple imputation based largely on the degree of elevation of dRVVT. At each visit, patients were classified into state 1 (a negative LAC), state 2 (a positive LAC), or state 3 (thrombosis). Multistate Markov models were used to provide estimates of relative transitions rates and to identify predictors in these transitions. The multiply imputed datasets were analyzed for complete data by imputation. Then, the results were pooled from the multiple analyses.
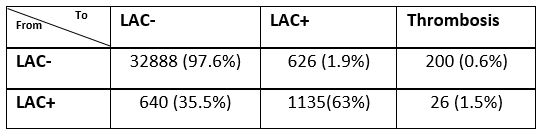
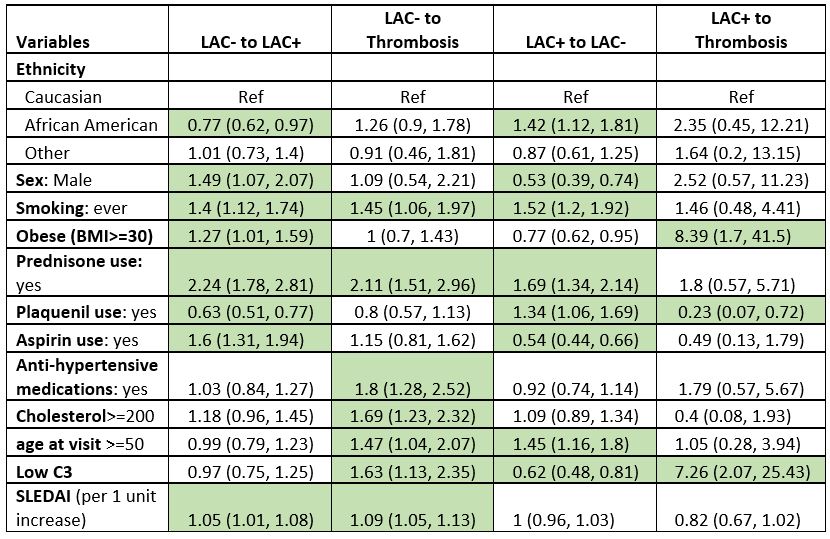
Results: 1781 patients (37296 clinic visits) were eligible to be included for this analysis. 93% were female, 41% were African American, 50% were Caucasian. The mean age at SLE diagnosis was 32 years (SD=13 years). Patients had the higher probability of improving (LAC+ to LAC-) than deteriorating (LAC- to LAC+), regardless of years after SLE diagnosis (Table 1, 2). In 5 years, the probability of remaining in the same state was 87.6% for state 1, and 4.6% for state 2. 7.7% of the patients initially in state 1 and 9.7% of the patients initially in state 2 transitioned to developing a thrombosis (Table 2). Multivariable regression results showed that African American ethnicity, normal C3, and being on hydroxychloroquine treatment were at higher rates of transitioning from positive LAC to negative LAC while male sex, SLEDAI, and obesity predicted higher rates of transition from LAC negative to positive states. For patients transitioning from positive LAC, obesity and low C3 levels were risk factors for thrombosis and being on hydroxychloroquine was protective against thrombosis (Table 3).
Conclusion: In SLE, transitions between LAC status could be estimated by multistate Markov model. We can estimate the risk of future thrombosis based on the baseline RVVT status, C3, ethnicity, gender, disease activity and obesity.
To cite this abstract in AMA style:
Demir S, Li J, Magder L, Petri M. Predicting the Transitions Between Lupus Anticoagulant Status and Thrombosis in SLE Using a Multi-state Markov Model [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/predicting-the-transitions-between-lupus-anticoagulant-status-and-thrombosis-in-sle-using-a-multi-state-markov-model/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predicting-the-transitions-between-lupus-anticoagulant-status-and-thrombosis-in-sle-using-a-multi-state-markov-model/