Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: The longitudinal experience of COVID-19 illness in patients with rheumatic diseases is emerging. Reports from the general population have described post-acute sequelae of SARS-CoV-2 (PASC) including de novo autoimmunity but evidence in patients with pre-existing rheumatic diseases is limited. We sought to characterize PASC in patients with rheumatic diseases in our majority Latino patient cohort. Further, we investigated the relationship between COVID-19 illness, the subsequent development of new autoantibodies, and increased rheumatic disease activity.
Methods: This is a retrospective study of patients with rheumatic diseases from an existing observational cohort, comprising of 72.4% Latino patients. Patients seen between April 1, 2020 to May 15, 2021 were included in analyses. We reviewed demographics, rheumatic disease, immunomodulatory therapies, and PASC symptoms. Antibodies to SARS-CoV-2 were measured for patients reporting infection. Antibodies to extractable nuclear antigens and anti-phospholipid antibodies were repeated once in the post-acute period when feasible. Data for continuous variables were expressed as the mean ± SD and categorical variables were summarized by computing counts of patients (%). Fisher’s exact test was used, and significance threshold was 0.05.
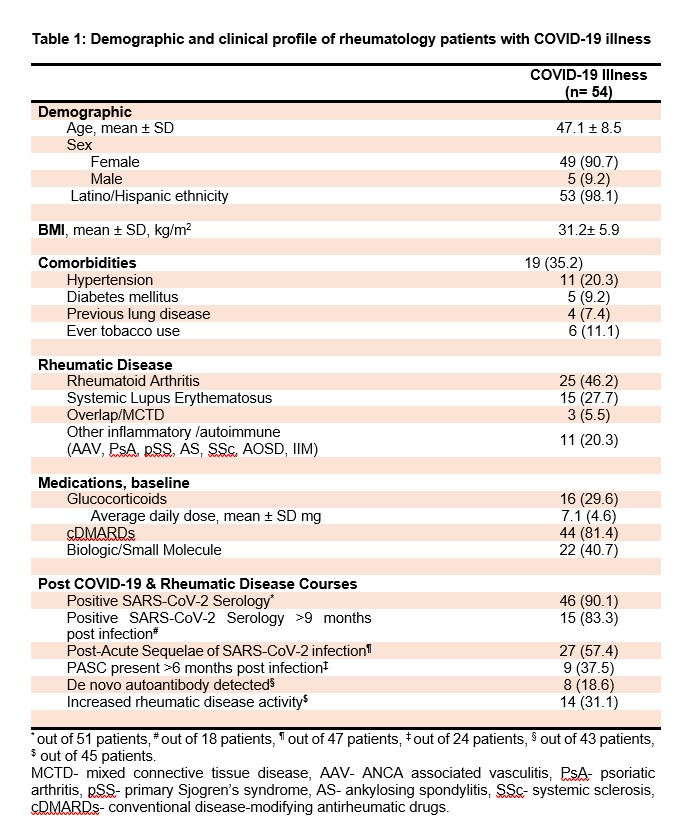
Results: During the study period, 54 patients reported COVID-19 illness, representing 17.5% of our cohort of 307 active patients (Table 1); 53 were Latino patients. Most patients had mild illness with 8 patients (14.8%) requiring inpatient management. There were no COVID-19 related deaths. SARS-CoV-2 IgG was assessed in sera in 52 individuals, and 5 patients (9.6%) were found to have negative titers while 83.3% of initially positive patients maintained their antibodies 9 months post infection. Of 47 patients assessed, 27 (57.4%) reported PASC symptoms and 24 of those patients (37.5%) had persistent PASC six months post infection. Autoantibody tests were performed in 39 patients after acute COVID-19 infection and a new autoantibody was detected in 8 patients (18.6%). Anti-RNP developed in 5 patients, anti-Scl70 in one patient, and anti-phospholipid antibodies in 2 patients. Subgroup analysis revealed a significantly higher frequency of autoantibody development in patients with RA when compared to other patients with COVID-19 (7/18 vs 1/21, p=0.01). This autoantibody development was higher than RA patients without COVID-19. The frequency of self-reported worsened rheumatic symptoms was higher among patients who developed a new autoantibody in the post-COVID-19 period than in other patients (6 of 8 vs 8 of 37, p=0.006).
Conclusion: Latino patients not only have an increased rate of COVID-19 infection but also shoulder an outsized burden of its post-acute sequelae. The finding of de novo autoantibody production in 18.6% of patients, post-COVID-19, could foretell the development of a new autoimmune phenomenon. Patients in high-risk groups for COVID-19, particularly marginalized groups, will require closer monitoring, early identification, and therapeutic intervention for detecting this new autoimmune phenotype. This likely will be an ongoing, long term effort.
To cite this abstract in AMA style:
Fike A, Pamuk O, Luo Y, Chu J, Ruiz-Perdomo Y, Hasni S, Gourh P, Katz J. Post-acute Sequelae of SARS-CoV-2 and Serological Response in a Cohort of Patients with Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/post-acute-sequelae-of-sars-cov-2-and-serological-response-in-a-cohort-of-patients-with-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/post-acute-sequelae-of-sars-cov-2-and-serological-response-in-a-cohort-of-patients-with-rheumatic-diseases/