Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Persistent presence of antiphospholipid antibodies (aPLs) are important thrombosis-related laboratory parameters, as well as an indication of anticoagulation use which usually cause higher bleeding risk. Cerebral microbleeds (CMBs) are strongly associated with both bleeding propensity and ischemic events. Till now, the correlation between aPLs and CMBs remained unclear.
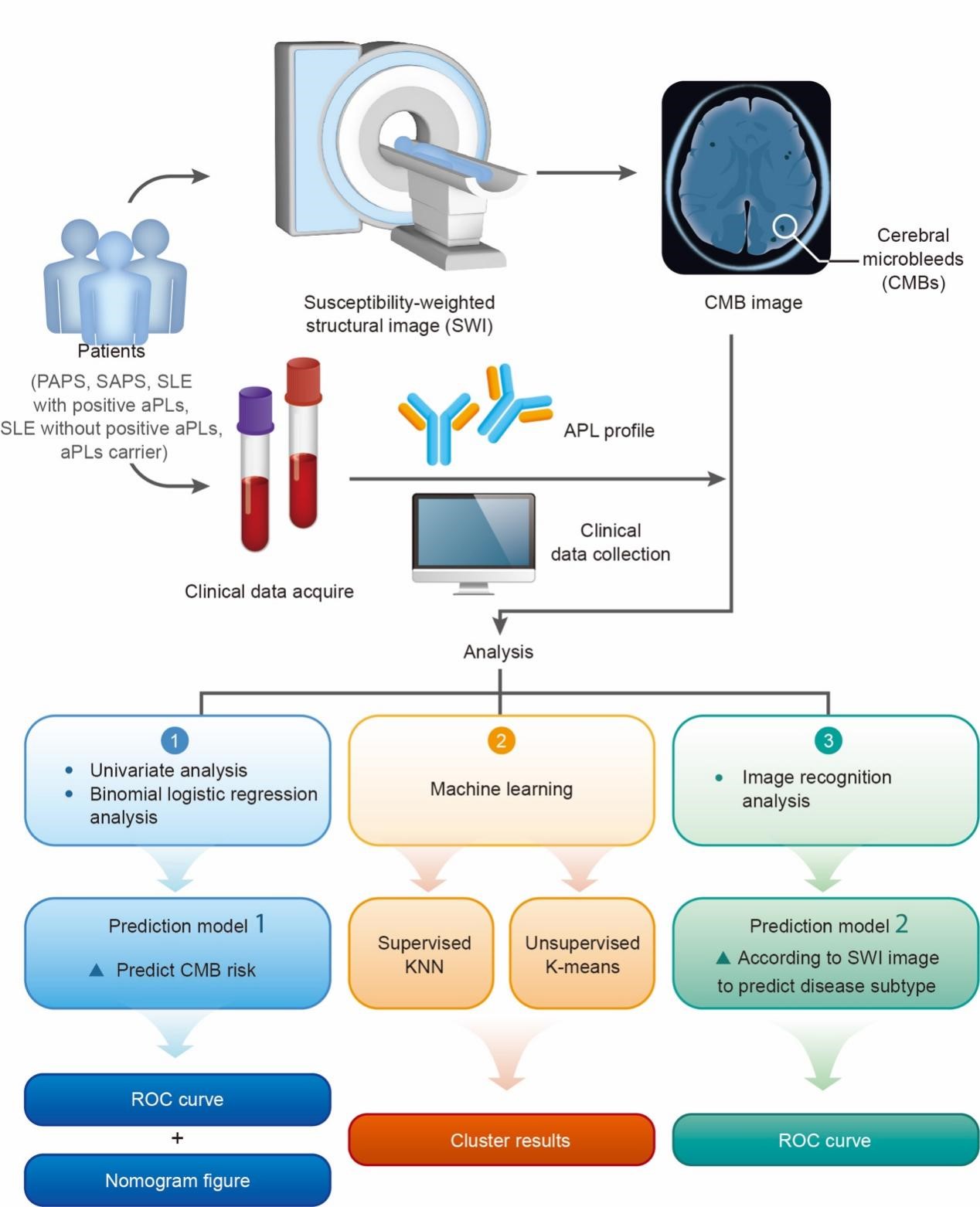
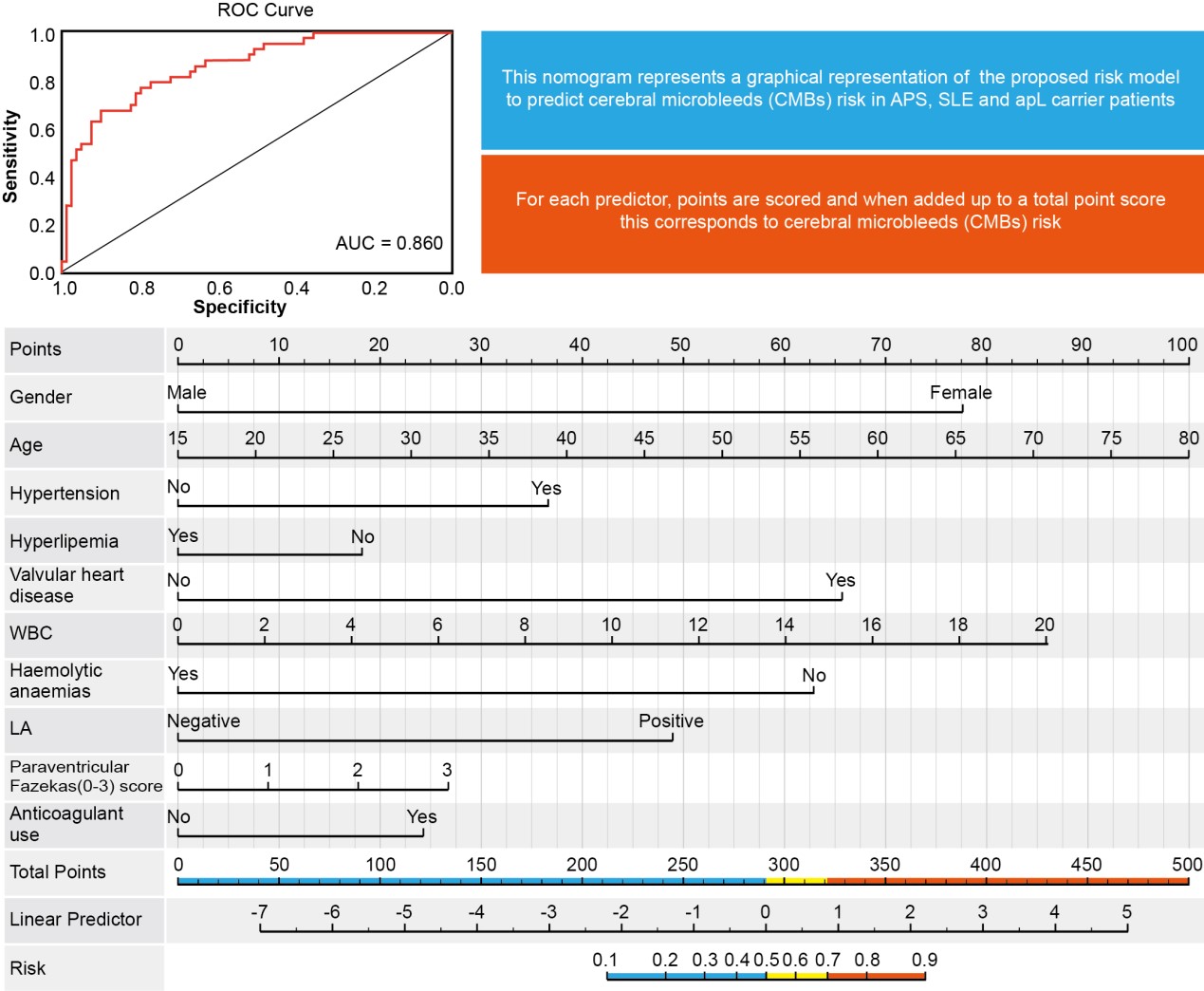
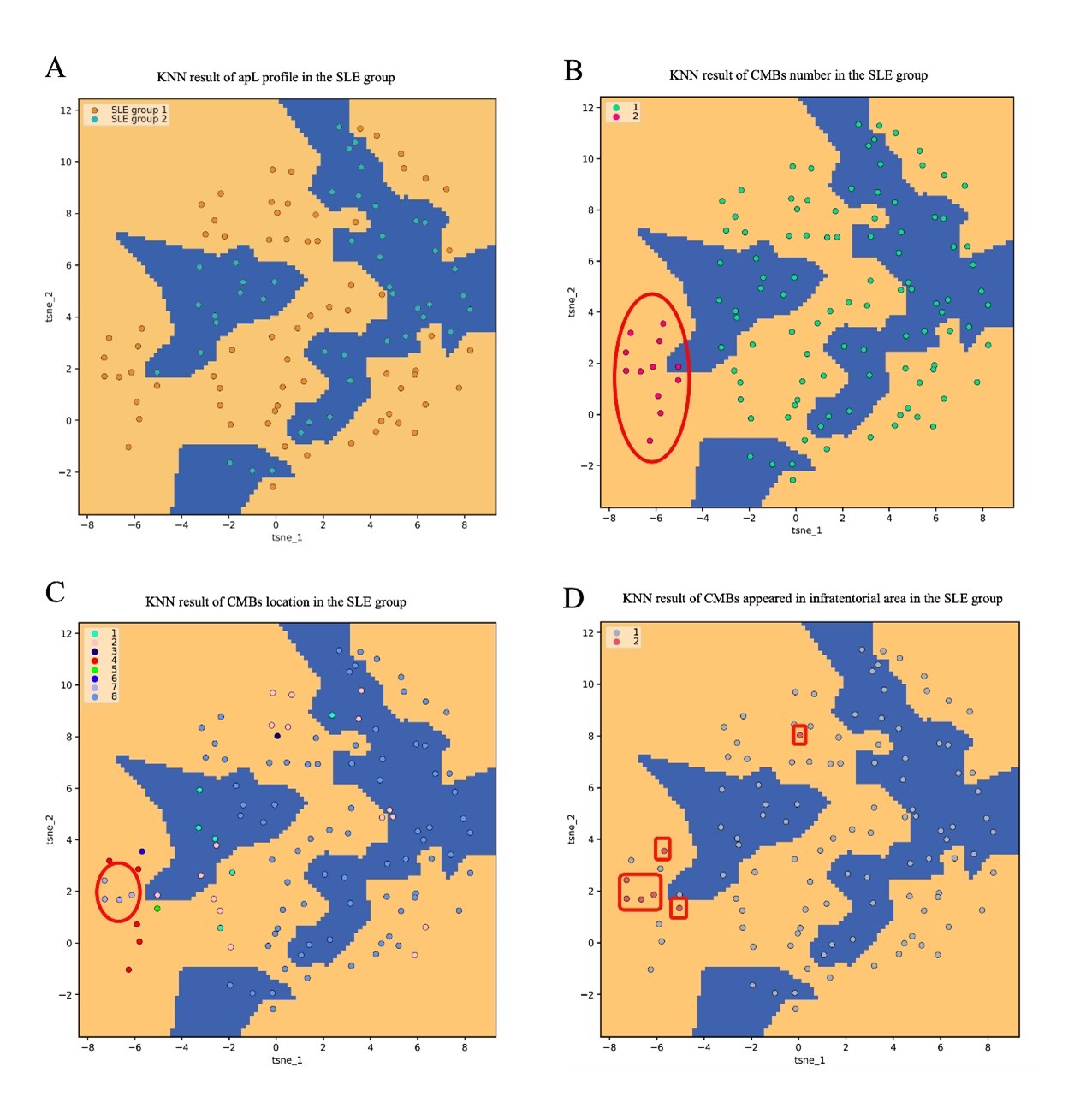
Methods: 31 primary antiphospholipid syndrome (APS), 50 secondary APS, 19 systemic lupus erythematosus (SLE) with positive aPLs, 44 SLE without positive aPLs and 16 aPLs carriers were enrolled from 2018 to 2021 in the Department of Rheumatology and Immunology in Ruijin Hospital. Clinical data, aPLs profile and susceptibility-weighted imaging(SWI) data were collected. Statistical analysis, machine learning, and image recognition analysis were performed from September 2022 to December 2022. Univariate and binomial logistic regression (prediction model 1) analysis was performed to investigate the risk factors of CMBs. Differences in CMBs between those with or without aPLs were analyzed by machine learning (supervised K-Nearest Neighbor (KNN) classification and unsupervised K-means clustering analysis) in SLE patients. Then, an image recognition analysis (prediction model 2) was conducted to build a model to predict the disease subtypes. Receiver operating characteristic (ROC) curve and nomogram representation of the binomial logistic regression analysis for CMBs risk and ROC curve of the image recognition analysis were set up. The area under the curve (AUC) was calculated to reflect the model performance. The results of machine learning were visualized by dimension reduction.
Results: Anti-cardiolipin antibody (aCL) IgG, lupus anticoagulant (LA), and apL-positive number showed a significant difference in the univariate analysis. In prediction model 1 (AUC=0.86), LA played an important role (p< 0.05, OR(95%CI): 1.31–13.24). The results of machine learning illustrated that SLE patients with positive aPLs had more CMBs numbers, more CMBs sites, and the possibility of infratentorial region hemorrhage. In addition, prediction model 2 (AUC=0.81) possessed good accuracy to predict the disease subtypes.
Conclusion: APLs were closely related to CMBs, of which LA played the most important role. It could be considered to screen CMBs by SWI in aPLs-positive patients.
Abbreviations: CMBs: Cerebral microbleeds; ROC: Receiver operating characteristic curve; AUC: Area under the curve; LA: Lupus anticoagulant.
Abbreviations: KNN: K-Nearest Neighbor; SLE: Systemic lupus erythematosus; aPLs: Antiphospholipid antibodies: SAPS: Secondary antiphospholipid syndrome; CMBs: Cerebral microbleeds.
To cite this abstract in AMA style:
Ye J, You Y, Zhou Z, wang F, Wu J, Yang C. Positive Antiphospholipid Antibodies Are Associated with a Higher Risk of Cerebral Microbleeds [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/positive-antiphospholipid-antibodies-are-associated-with-a-higher-risk-of-cerebral-microbleeds/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/positive-antiphospholipid-antibodies-are-associated-with-a-higher-risk-of-cerebral-microbleeds/