Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a complex chronic heterogeneous autoimmune disease, which increases the risk of atherothrombosis. In addition to their well described role in thrombosis and hemostasis, platelets are key mediators of inflammation and have immune effector cell properties. This study was initiated to investigate the role of platelet associated Lectin Galactoside-binding Soluble 3 Binding Protein (LGALS3BP), which binds to macrophage-associated lectin Mac-2, as a mediator of inflammation in SLE and potential biomarker associated with clinical phenotypes.
Methods: RNA transcriptome analysis was performed on platelets isolated from 51 patients with SLE (not taking aspirin or anticoagulants) and 18 age, sex and race/ethnicity matched controls. LGALS3BP protein expression was determined in platelet releasates by ELISA and western blot analysis. Gene and protein expression of LGALS3BP in Megakaryocyte cell line (MEG-01) was investigated upon stimulation with IFN-ɑ. Correlations between circulating serum LGALS3BP and LGALS3BP platelet mRNA and releasates were assessed. Subsequently, correlation analysis between clinical features of SLE and circulating serum LGLAS3BP was performed. Finally, the effects of platelets and LGALS3BP on macrophage inflammatory response were studied in vitro.
Results: Platelet transcriptome analysis revealed that LGALS3BP was one of the most differentially expressed transcripts in SLE versus matched-healthy controls (Fold change, 3.9, adjusted P-value = 2.5 x 10-11) (Figure1A). Consistently, LGALS3BP in platelet releasates was significantly higher in 40 patients with SLE than 20 controls (p = 0.002) (Figure1B). Platelet LGALS3BP gene and protein expression were highly correlated with circulating LGALRS3BP in serum (r2 = 0.370, p = 0.003 and r2 = 0.689, p < 0.0001 respectively) (Figure1E and F). LGALS3BP measured in serum of 115 patients with SLE correlated with the SELENA SLEDAI hybrid disease activity index (r2= 0.322, p = 0.0005) (Figure1G). In particular, higher serum LGALS3BP levels were observed in SLE patients with lupus nephritis compared to those with SLE and inactive disease (P=0.0001) (Figure1H). In longitudinal analysis of 22 patients without proteinuria at baseline who went on to develop proteinuria over time, circulating plasma LGALS3BP tracked with flares of nephritis (p=0.06). In vitro, IFN-α induced the expression and production of LGALS3BP in MEG-01 cells in a dose dependent manner (Figure2A, B and C), which was completely inhibited by IFN-α neutralizing antibody (Figure2D, E and F). Recombinant LGALS3BP (Figure 3A and B) and Platelet releasates from SLE (Figure 3C) induced the production of pro-inflammatory cytokines such as IL-8 (p=0.04) and IL-6 (p=0.073) by macrophages.
Conclusion: These data show that platelets isolated from patients with SLE highly express and secrete LGALS3BP which induces a proinflammatory macrophage and is associated with SLE disease clinical phenotype. LGALS3BP may contribute to pathogenesis and serve as a novel biomarker of SLE disease activity.
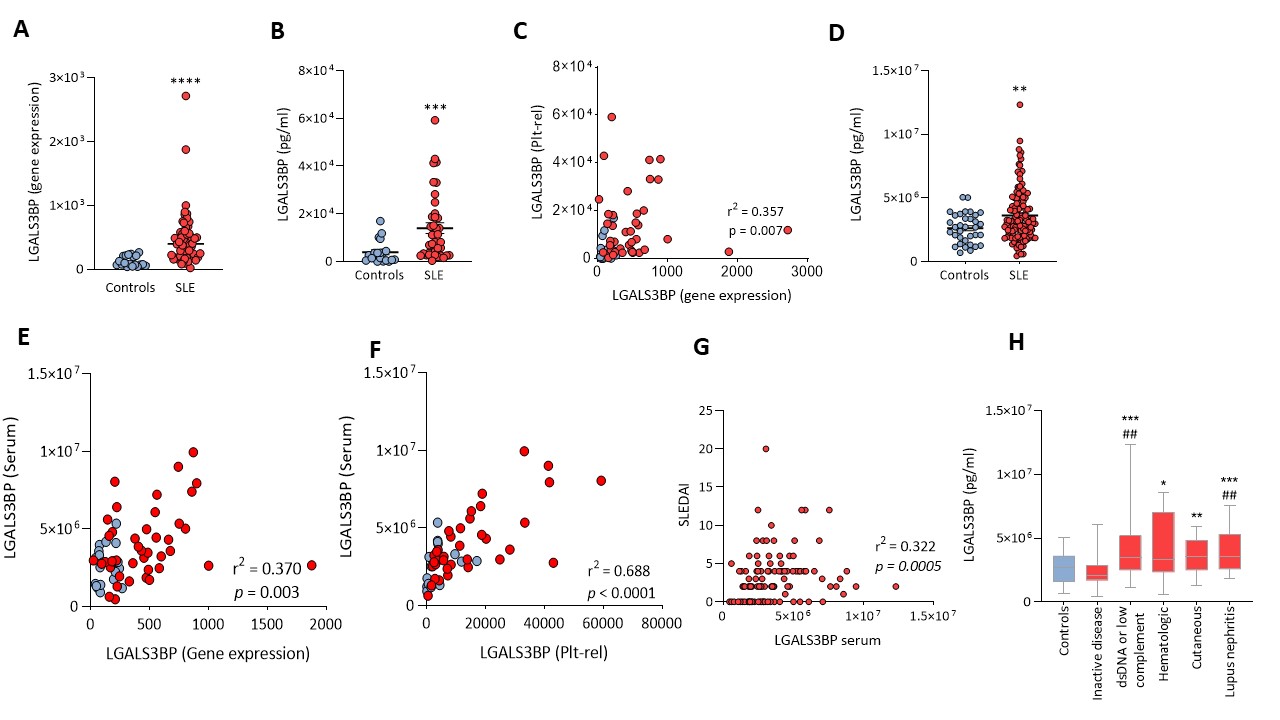 Figure 1: LGALS3BP is highly expressed in SLE and correlates with SELENA SLEDAI hybrid disease activity index A) LGALS3BP gene expression in platelets isolated from 51 patients with SLE and 18 age, sex and race/ethnicity matched controls, determined by RNA sequencing analysis. B) Levels of LGALS3BP measured by LGALS3BP specific ELISA in platelet releasates (plt-rel) of 40 patients with SLE and 20 healthy controls. C) Correlation between the levels of LGALS3BP measured in platelet releasates and platelet LGALS3BP gene expression D) LGALS3BP levels measured by LGALS3BP specific ELISA in serum of 115 patients with SLE and 34 healthy controls. E) Correlation between serum LGALS3BP and Platelet LGALS3BP gene expression F) Correlation between serum LGALS3BP and LGALS3BP in platelet releasates in 36 patients with SLE and 16 healthy controls G) Correlation between serum LGALS3BP levels and SELENA SLEDAI hybrid disease activity index in 115 patients with SLE H) Serum LGALS3BP levels stratified based on clinical phenotypes. Pounds indicate comparison to healthy controls and asterisks to inactive disease All data represent the mean ± s.e.m. and are analyzed by two-sided Student’s t-test. *P
Figure 1: LGALS3BP is highly expressed in SLE and correlates with SELENA SLEDAI hybrid disease activity index A) LGALS3BP gene expression in platelets isolated from 51 patients with SLE and 18 age, sex and race/ethnicity matched controls, determined by RNA sequencing analysis. B) Levels of LGALS3BP measured by LGALS3BP specific ELISA in platelet releasates (plt-rel) of 40 patients with SLE and 20 healthy controls. C) Correlation between the levels of LGALS3BP measured in platelet releasates and platelet LGALS3BP gene expression D) LGALS3BP levels measured by LGALS3BP specific ELISA in serum of 115 patients with SLE and 34 healthy controls. E) Correlation between serum LGALS3BP and Platelet LGALS3BP gene expression F) Correlation between serum LGALS3BP and LGALS3BP in platelet releasates in 36 patients with SLE and 16 healthy controls G) Correlation between serum LGALS3BP levels and SELENA SLEDAI hybrid disease activity index in 115 patients with SLE H) Serum LGALS3BP levels stratified based on clinical phenotypes. Pounds indicate comparison to healthy controls and asterisks to inactive disease All data represent the mean ± s.e.m. and are analyzed by two-sided Student’s t-test. *P
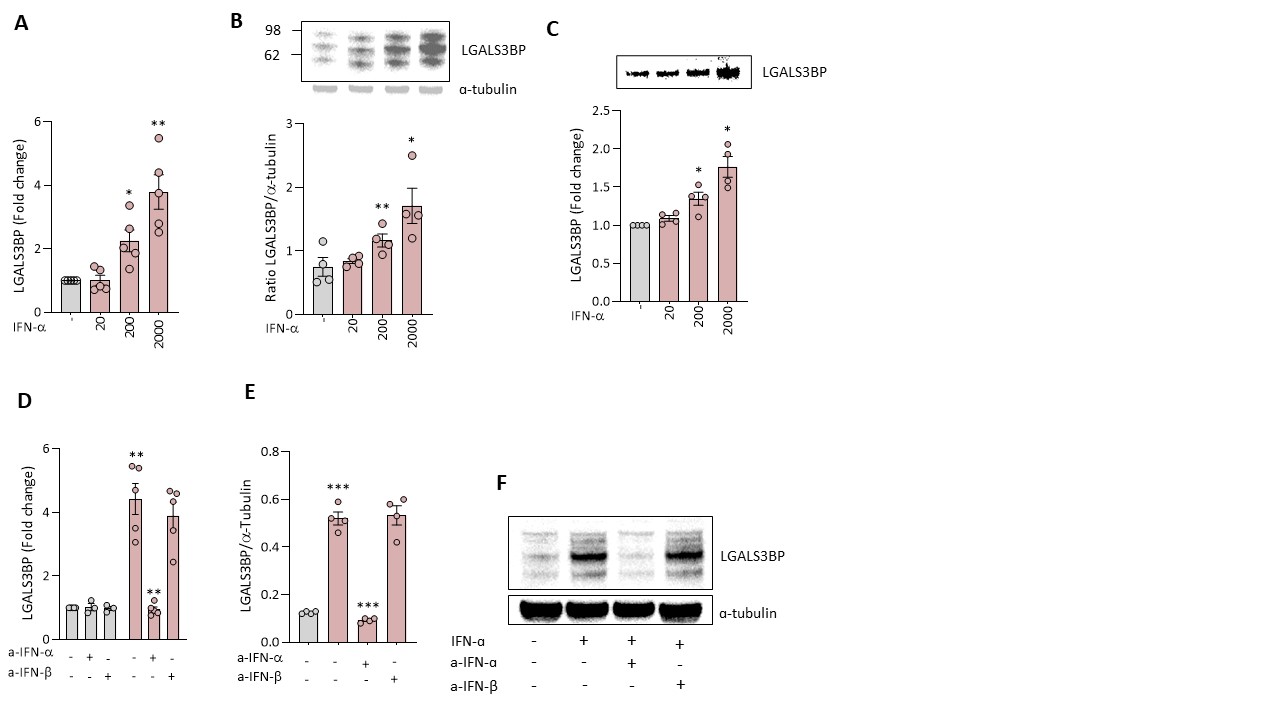 Figure 2: IFN-ɑ induces the expression and the production of LGALS3BP in Megakaryocyte cell line (MEG-01) in a dose dependent manner MEG-01 cells were stimulated or not with 20, 200 and 2000 U/mL IFN-ɑ. After 24h, LGALS3BP gene expression (A) and protein expression in the lysates and supernatants (B and C respectively) were determined by qPCR and western blot analysis. LGALS3BP gene (D) and protein (E and F) expression were quantified using qPCR and western blot in MEG-01 cell lysates after stimulation with 2000 U/mL IFN-ɑ in the presence or absence of neutralizing antibodies against IFN-ɑ and IFN-β All data represent the mean ± s.e.m. and are analyzed by two-sided Student’s t-test. *P
Figure 2: IFN-ɑ induces the expression and the production of LGALS3BP in Megakaryocyte cell line (MEG-01) in a dose dependent manner MEG-01 cells were stimulated or not with 20, 200 and 2000 U/mL IFN-ɑ. After 24h, LGALS3BP gene expression (A) and protein expression in the lysates and supernatants (B and C respectively) were determined by qPCR and western blot analysis. LGALS3BP gene (D) and protein (E and F) expression were quantified using qPCR and western blot in MEG-01 cell lysates after stimulation with 2000 U/mL IFN-ɑ in the presence or absence of neutralizing antibodies against IFN-ɑ and IFN-β All data represent the mean ± s.e.m. and are analyzed by two-sided Student’s t-test. *P
 Figure 3: LGALS3BP and platelets from patients with SLE induce production of pro-inflammatory cytokines IL-8 and IL-6 in macrophages Monocytes derived macrophages were cultured for 7 days for differentiation in the presence of macrophage colony stimulating factor (MCSF) After differentiation, cells were either cultured without stimulation or stimulated with increasing concentrations of LGALS3BP (2.5, 10 and 40 μg/mL) for 6h and cytokine gene expression (A) and secretion (B) were determined by qPCR and multiplex beads-based assay respectively. Platelet releasates from patients with SLE or healthy controls were added to macrophages for 24h. IL-8 and IL-6 were measured in the supernatants using multiplex beads-based assay respectively. All data represent the mean ± s.e.m. and are analyzed by two-sided Student’s t-test. *P
Figure 3: LGALS3BP and platelets from patients with SLE induce production of pro-inflammatory cytokines IL-8 and IL-6 in macrophages Monocytes derived macrophages were cultured for 7 days for differentiation in the presence of macrophage colony stimulating factor (MCSF) After differentiation, cells were either cultured without stimulation or stimulated with increasing concentrations of LGALS3BP (2.5, 10 and 40 μg/mL) for 6h and cytokine gene expression (A) and secretion (B) were determined by qPCR and multiplex beads-based assay respectively. Platelet releasates from patients with SLE or healthy controls were added to macrophages for 24h. IL-8 and IL-6 were measured in the supernatants using multiplex beads-based assay respectively. All data represent the mean ± s.e.m. and are analyzed by two-sided Student’s t-test. *P
To cite this abstract in AMA style:
EL Bannoudi H, Cornwell M, Luttrell-Williams E, Engel A, Rolling C, Izmirly P, Belmont H, Ruggles K, Clancy R, Buyon J, Berger J. Platelet Secreted LGALS3BP Induces a Pro-inflammatory Phenotype in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/platelet-secreted-lgals3bp-induces-a-pro-inflammatory-phenotype-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/platelet-secreted-lgals3bp-induces-a-pro-inflammatory-phenotype-in-systemic-lupus-erythematosus/
