Session Information
Date: Sunday, November 12, 2023
Title: Abstracts: RA – Diagnosis, Manifestations, & Outcomes I: RA-ILD
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Matrix metalloproteinases (MMPs) are enzymes involved in extracellular matrix remodeling that have been implicated in the pathogenesis and progression of rheumatoid arthritis (RA) and interstitial lung diseases (ILD). We aimed to assess the associations of plasma MMPs with the presence and severity of RA-ILD, as well as RA-ILD sub-groups defined by imaging and genetic risk.
Methods: We performed a cross-sectional study of participants with/without ILD in the Veterans Affairs Rheumatoid Arthritis registry, a multicenter prospective cohort of U.S. Veterans with RA. Participants who developed ILD after registry enrollment were excluded. Prevalent ILD diagnoses were systematically validated through medical record review of clinical diagnoses, imaging findings, and biopsy reports. Imaging pattern was classified as usual interstitial pneumonia (UIP) when documented in the clinical read or if honeycombing was present vs. non-UIP for all others. Plasma MMP-1, -3, -7, and -9 concentrations (MesoScale Discovery platform) and the MUC5B rs35705950 promoter variant (Illumina Infinium Global Screening Array) were measured on plasma and DNA samples, respectively, collected at enrollment. MMP values were log-transformed, standardized, and categorized into quartiles. The most proximate forced vital capacity (FVC) result within three years of registry enrollment was collected from the electronic health record. Associations of MMPs with prevalent RA-ILD were assessed with logistic regression models adjusted for age, sex, race, smoking status, anti-CCP positivity, and RA disease activity. Associations of MMP values with FVC were assessed with Pearson’s correlation coefficient. MMP values were compared across MUC5B genotypes (positive vs. negative) and ILD patterns using Kruskal-Wallis tests. In sensitivity analyses, we included RA-ILD cases developing within one year after enrollment given disease latency.
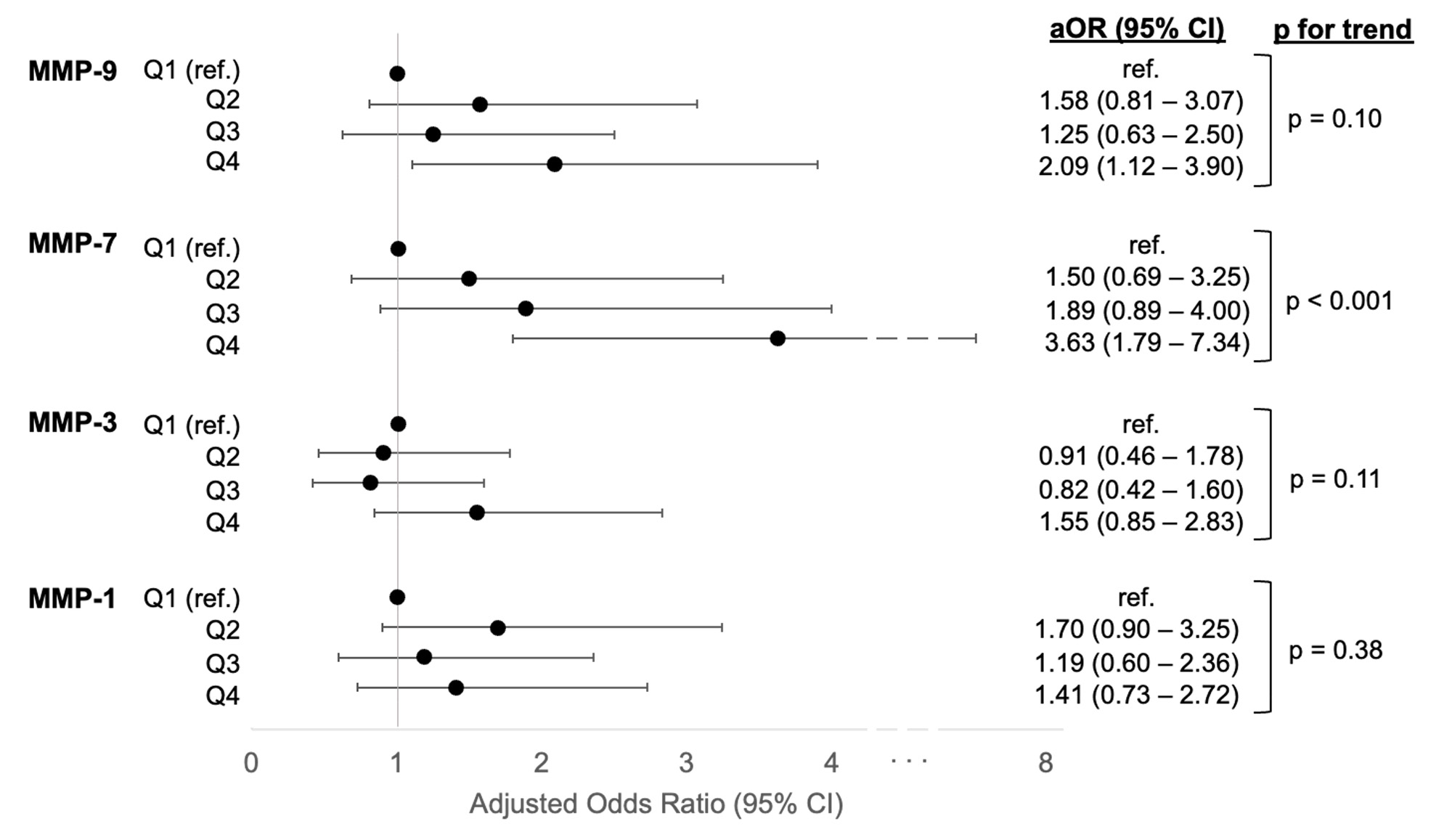
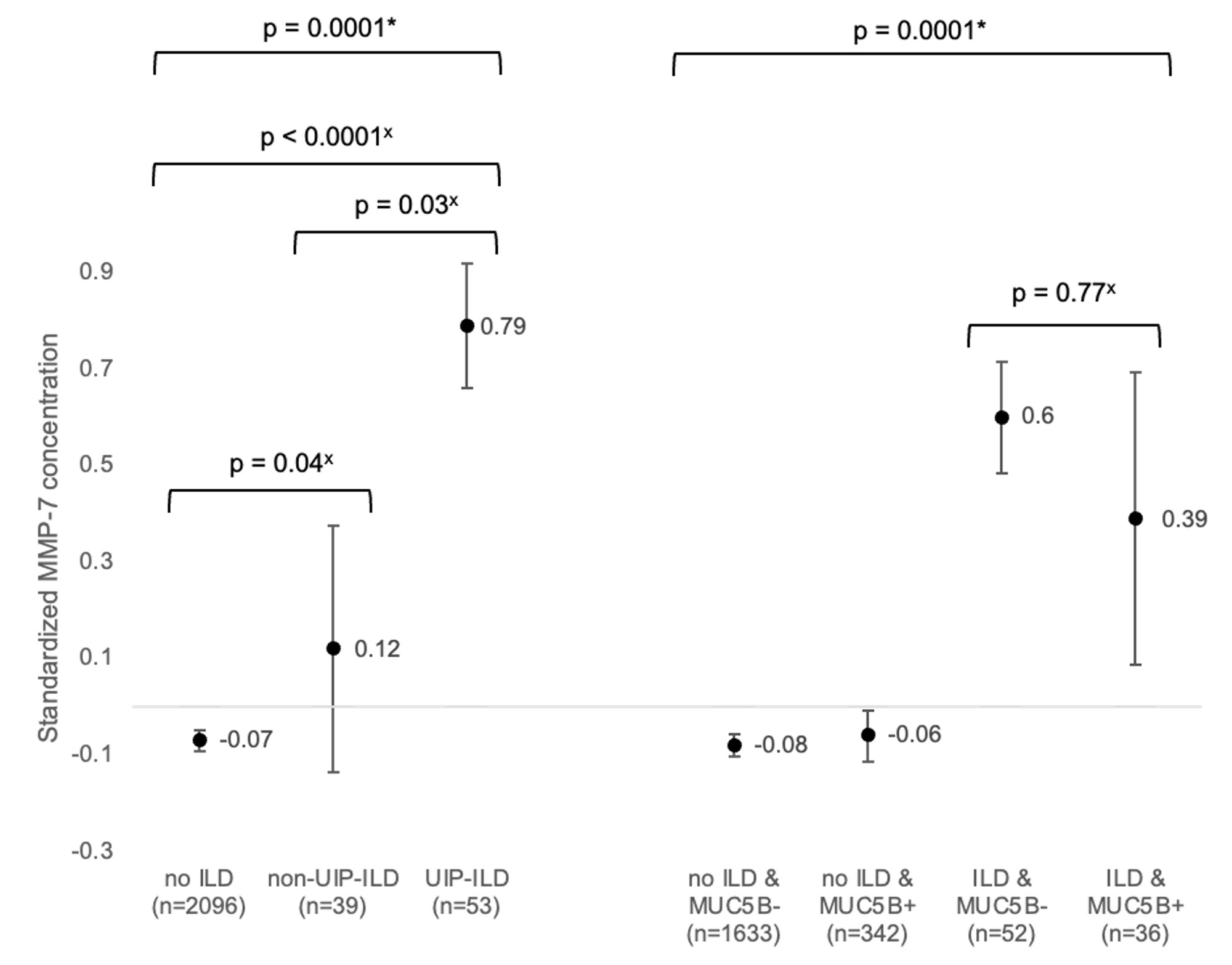
Results: Among 2,189 participants (89% male, mean age 64 years), RA-ILD was present in 93 at the time of registry enrollment (point prevalence 4.2%). Higher plasma concentrations of MMP-7 (OR 1.64 [95% CI 1.31, 2.05] per standardized unit) and MMP-9 (OR 1.27 [1.01, 1.59]) were significantly associated with prevalent RA-ILD, but MMP-1 and -3 were not. Participants with the highest quartile of MMP-7 had over 3 times the odds of prevalent RA-ILD (OR 3.63 [1.80, 7.34], Figure 1) compared to the lowest quartile. The highest quartile of MMP-9 was also associated with >2-fold higher odds of RA-ILD. MMP-9 concentrations, but not other MMPs, were weakly negatively correlated with FVC (r = -0.28, p = 0.015) among those with ILD. MMP-7 was higher among participants with a UIP vs. non-UIP pattern (Figure 2). MMP concentrations did not differ by the presence of the MUC5B promoter variant (MMP-7 shown in Figure 2). Similar results were observed in sensitivity analyses (data not shown).
Conclusion: Plasma concentrations of MMP-7/9 were strongly associated with prevalent RA-ILD, which was largely driven by patients with a UIP pattern of ILD. MMP-9, but not MMP-7, was weakly correlated with RA-ILD severity by FVC. These findings add to a growing body of literature suggesting MMPs may have a potential pathogenic role in RA-ILD.
Odds ratio adjusted for age, sex, race, smoking status, anti-citrullinated peptide antibody status, and rheumatoid arthritis disease activity in logistic regression model. Quartile 1 (referent) was the lowest values. Abbreviations: MMP = matrix metalloproteinase, ILD = interstitial lung disease, RA = rheumatoid arthritis, aOR = adjusted odds ratio, ref. = referent.
Standardized values of log-transformed MMP-7 concentrations were calculated by subtracting the sample mean value and dividing by the standard deviation. Error bars indicate standard error of the mean.
*across entire sample by Kruskal-Wallis test
x pairwise comparison by post hoc Dunn test
Abbreviations: MMP = matrix metalloproteinase, ILD = interstitial lung disease, UIP = usual interstitial pneumonia
To cite this abstract in AMA style:
Luedders B, Wheeler A, Ascherman D, Baker J, Duryee M, Yang Y, Roul P, Wysham K, Monach P, Reimold A, Kerr G, Kunkel G, Cannon G, Poole J, Thiele G, Mikuls T, England B. Plasma Matrix Metalloproteinases in Rheumatoid Arthritis-Interstitial Lung Disease: Associations with Disease Presence, Severity, and Subtypes [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/plasma-matrix-metalloproteinases-in-rheumatoid-arthritis-interstitial-lung-disease-associations-with-disease-presence-severity-and-subtypes/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/plasma-matrix-metalloproteinases-in-rheumatoid-arthritis-interstitial-lung-disease-associations-with-disease-presence-severity-and-subtypes/