Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: MMF is a key therapy for moderate to severe SLE. MMF inhibits inosine monophosphate dehydrogenase, an enzyme needed in nucleotide synthesis required for lymphocyte proliferation. MMF can also inhibit B-cell activation and plasma cell differentiation. Antibody production, interferon elevation, dysregulated inflammatory soluble mediators, and altered lymphocyte activity are molecular features of SLE. One soluble mediator, stem cell factor (SCF), was recently noted to be elevated in patients who transitioned from pre-SLE to SLE. Examination of cellular activity in patients undergoing MMF therapy may elucidate ongoing immune processes in patients who fail to respond, as up to 50% of MMF-treated LN patients are non-responders.
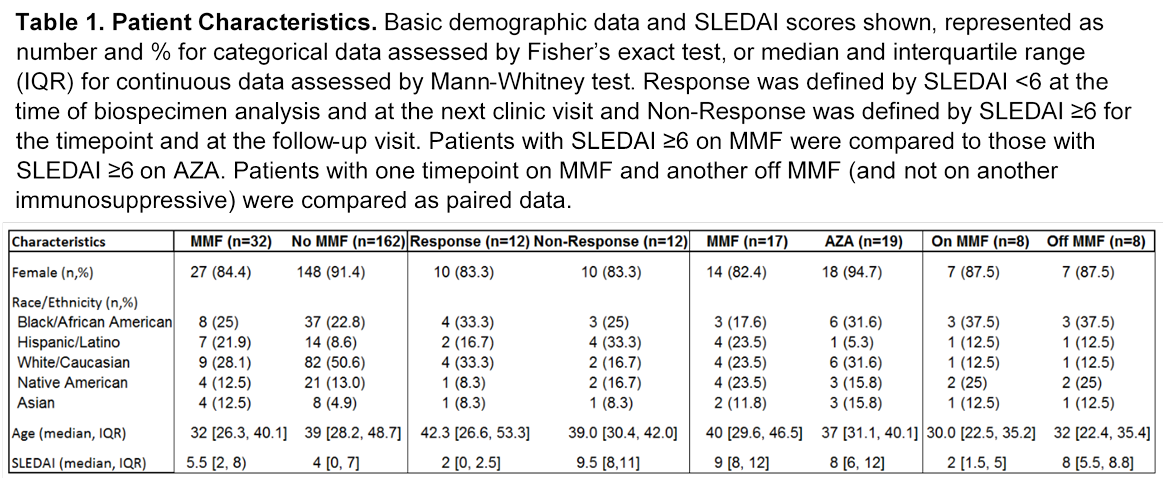
Methods: Immunologic profiling was conducted on 194 patients who met ACR classification criteria for SLE. Molecular assessments included whole blood gene expression profiling (microarray, analyzed as modules normalized to healthy controls, described by Chaussabel) and plasma soluble mediator assessment (24 cytokines, chemokines, and soluble receptors which passed quality control). We used these data for 3 key analyses. Patients who demonstrated clinical response to MMF (n=12) were compared to those with inadequate response (n=12). High disease activity (SLEDAI ≥ 6) patients on MMF (n=17) were compared to those on AZA (n=19). Wilcoxan test was used to analyze patients with one visit while taking MMF and another while not receiving MMF (n=8 pairs) (Table 1).
Results: The patients in the cohort whose biospecimens were assayed while on MMF (n=32) were younger (p=0.01) and had more Hispanic and Asian patients with less white patients (p=0.04) than those without MMF exposure (n=162). No significant differences in gender, race, or age were present between the other comparison groups. Plasma cell downregulation differentiated responders from non-responders and T-cell downregulation differentiated MMF from AZA treated patients. MMF was less effective at controlling elevated interferon and elevated SCF than AZA (Figure 1). Additionally, in the paired data, monocyte chemoattractant protein 1 was lower while on MMF as compared to off (p=0.04, not shown).
Conclusion: In this translational study of SLE, we showed that resistance to plasma cell suppression in some patients likely contributed to their ineffective MMF treatment. Also, we demonstrated that MMF differentially modulated T-Cell and IFN pathways compared to AZA. Understanding these distinct molecular profiles responding to MMF and AZA can lead to more effective personalized combination therapies.
To cite this abstract in AMA style:
Arriens C, Lu R, Aberle T, Kamp S, DeJager W, Munroe ME, Chakravarty E, Thanou K, Merrill JT, Guthridge JM, James JA. Plasma Cell and T-Cell Activity Downregulation during MMF Therapy in SLE May be Necessary for Successful Immunosuppression [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/plasma-cell-and-t-cell-activity-downregulation-during-mmf-therapy-in-sle-may-be-necessary-for-successful-immunosuppression/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/plasma-cell-and-t-cell-activity-downregulation-during-mmf-therapy-in-sle-may-be-necessary-for-successful-immunosuppression/