Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Varicella-zoster virus(VZV) or Shingles infections in immunocompromised individuals can lead to severe complications. Despite availability of the Recombinant Varicella Zoster vaccine(RZV), vaccination rates remain suboptimal. The purpose of this research is to conduct a survey to assess physicians’ attitudes, knowledge, and practices regarding the RZV.
Methods: This was a cross-sectional survey conducted using an online platform from a diverse sample of physicians caring for immunocompromised patients (e.g., rheumatology, hematology-oncology, gastroenterology, transplant nephrology, infectious disease), with a special focus on those that prescribe JAK inhibitors (JAKi)
The survey instrument was developed based on a comprehensive literature review and consisted of the following sections:
-
Demographic and practice characteristics
-
Knowledge and awareness about the shingles vaccine
-
Attitudes and beliefs regarding the shingles vaccine
-
Vaccine recommendation and administration practices
Perceived barriers and facilitators to shingles vaccine uptake
The survey included a combination of multiple-choice questions, Likert-scale items, and open-ended questions to capture both quantitative and qualitative data
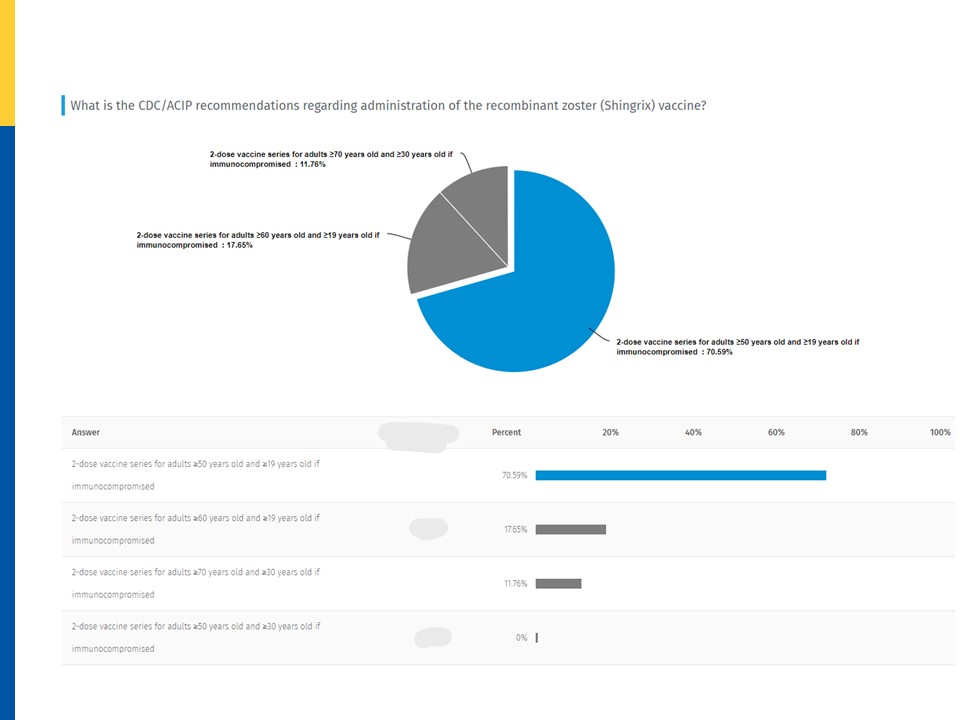
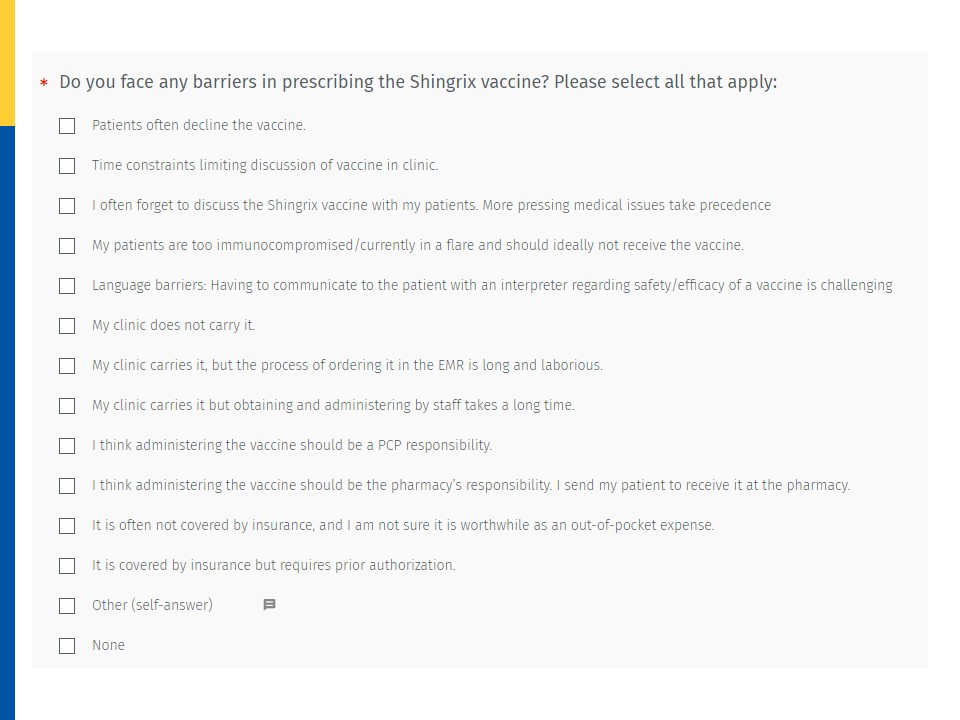
Results: The survey received 34 responses. The majority of respondents (53%) were between 30-39 years of age. Attending physicians constituted a larger proportion (83%) of the respondents compared to fellows (17%). The respondents predominantly specialized in rheumatology, infectious diseases, and hematology-oncology. Regarding knowledge of the CDC/ACIP recommendations for RZV, 71% of respondents demonstrated accurate understanding. When asked about their vaccine recommendation practices, 47% of physicians reported almost always recommending the RZV to their patients. The patient’s current health status, particularly the relative degree of immunosuppression, emerged as the most influential factor in the decision to recommend the vaccine. The top three barriers to prescribing the RZV were identified as follows: 1) patient reluctance to accept the vaccine, 2) time constraints limiting discussion of the vaccine during clinic visits, and 3) forgetting to discuss the RZV with patients due to prioritization of more pressing medical issues. All respondents (100%) reported feeling confident in the effectiveness and safety of the RZV. 62% of respondents answered that an appointment to return and receive the second dose was provided during the first visit itself. The study aimed to investigate a subgroup of physicians who frequently prescribe Janus kinase (JAK) inhibitors to patients with autoimmune conditions. The subgroup of physicians who prescribe JAKi was limited to only 7 physicians. Among these respondents, 70% reported being aware that JAK inhibitors may increase the risk of herpes zoster.
Conclusion: We suggest including patient handouts in the clinic area and incorporating such information in the after visit communication . By identifying potential barriers, facilitators, and knowledge gaps, this study aims to provide valuable insights that can inform interventions to enhance RZV uptake.
To cite this abstract in AMA style:
sutton c, wang y, iyer p. Physician Knowledge, Attitudes and Perceived Barriers to Recommending the Recombinant Varicella Zoster Vaccine [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/physician-knowledge-attitudes-and-perceived-barriers-to-recommending-the-recombinant-varicella-zoster-vaccine/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/physician-knowledge-attitudes-and-perceived-barriers-to-recommending-the-recombinant-varicella-zoster-vaccine/