Session Information
Date: Monday, October 22, 2018
Title: 4M084 ACR Abstract: Pediatric Rheum–Clinical I: Outcomes & Comorbidities (1846–1851)
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Juvenile myositis (JM) is an inflammatory disease that causes muscle weakness, skin rashes, and significant deconditioning. Little is known about long-term resolution of physical disability. We examined trajectories of physical function in JM.
Methods:
JM registry data were collected at routine visits (January 2000 to June 2014) to Ann & Robert H. Lurie ChildrenÕs Hospital of Chicago and analyzed in this study. Only patients whose baseline visit was < 3 months after initiation of treatment were included. The following variables were extracted: parent-proxy reported Childhood Health Assessment Questionnaire (CHAQ), gender, race, duration of untreated disease, Disease Activity Score (DAS) – muscle/skin domains, Childhood Myositis Assessment Scale (CMAS), muscle enzymes, nailfold capillary end row loops (NFC-ERL), von Willebrand factor antigen (vWFAg), calcinosis (ever experienced), lipodystrophy (ever experienced), TNFalpha-308A allele, and treatments. Descriptive statistics were calculated. Latent trajectory analysis was performed assessing probability of CHAQ > 0 (binary outcome 0 vs > 0). Baseline values for demographic/clinical variables above were compared across identified trajectories (FisherÕs exact; Kruskal-Wallis).
Results:
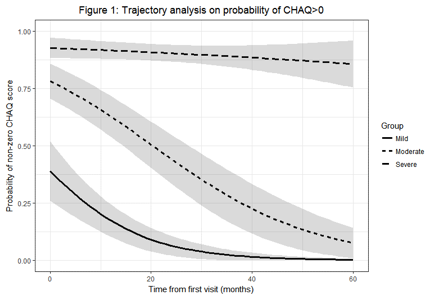
Baseline descriptive statistics for n = 104 included patients with median 13.5 study visits and median follow-up 54 months are shown in Table 1. Three trajectories corresponding to mild (n = 46 [44%]), moderate (n = 32 [31%]), and severe disability (n = 26 [25%]) were identified (Figure 1). Statistically significant differences in baseline variables for mild vs moderate vs severe groups were noted for: CHAQ (0.13 vs 0.88 vs 1.35, p < 0.001), DAS-Muscle (4 vs 6 vs 6, p = 0.001), and CMAS (40 vs 31 vs 34, p = 0.01). Median baseline NFC-ERL differed, with higher counts in the mild group (= 5) vs moderate and severe groups (= 3.83 and 4.14), p = 0.047. Race trended toward significance (p = 0.08), with fewer white patients in the severe group (n = 13 white patients vs n = 26 total patients in severe group).
Conclusion:
To our knowledge, this is the first study describing longitudinal trajectories of physical function (distinct from disease activity) in JM. Baseline physical function (i.e. CHAQ) and muscle weakness (i.e. DAS-Muscle, CMAS) predict long-term physical function trajectory. Baseline vasculopathy (i.e. NFC-ERL) may be less prominent in JM patients following the mild physical function trajectory. There may also be racial disparities in physical function trajectories among youth with JM, though this requires further study.
|
Table 1: Baseline Demographic and Clinical Descriptives (n = 104 patients)
|
||
|
n = # with baseline data
|
n (%) / median (IQR)
|
|
|
Race
|
104 |
|
|
White |
71 (68.3%) |
|
|
Hispanic |
20 (19.2%) |
|
|
Black |
7 (6.7%) |
|
|
Other* |
6 (5.8%) |
|
|
Female Gender
|
104 |
78 (75%) |
|
Age of Onset (years)
|
104 |
5.3 (2.7-7.7) |
|
Age at Initial Visit (years)
|
104 |
5.85 (3.6-8.2) |
|
Duration of Untreated Disease (months)
|
104 |
5.5 (2.4-11.9) |
|
CHAQ summary score value
|
101 |
0.62 (0.12-1.37) |
|
CHAQ summary score > 0
|
101 |
76 (75.2%) |
|
DAS-Skin
|
102 |
6 (5-6) |
|
DAS-Muscle
|
102 |
5 (3-7) |
|
CMAS
|
67 |
37 (30.5-44) |
|
AST
|
86 |
41 (30-63.3) |
|
CPK
|
90 |
106 (54.3-379.3) |
|
LDH
|
88 |
306 (243.8-463.5) |
|
Aldolase
|
86 |
10.2 (7.2-14.7) |
|
NFC-ERL
|
91 |
4.3 (3.7-5.6) |
|
vWF Ag (abnormal value)
|
87 |
67 (77%) |
|
Calcinosis (ever experienced)
|
104 |
9 (8.7%) |
|
Lipodystrophy (ever experienced)
|
104 |
31 (29.8%) |
|
TNFalpha-308A Allele
|
100 |
|
|
AA |
1 (1%) |
|
|
GA |
29 (29%) |
|
|
GG |
70 (70%) |
|
|
Medications:
|
|
|
|
On any medication at initial visit |
90 |
52 (57.8%) |
|
Oral or IV Steroids |
101 |
42 (41.6%) |
|
Methotrexate |
101 |
29 (28.7%) |
|
Other treatment (IVIG, etc)
|
55 |
15 (27.3%) |
|
*Other race group comprised of: 3 Asian, 1 ÔIndianÓ, 1 American Indian/Alaskan, and 1 ÔOtherÕ patient |
||
To cite this abstract in AMA style:
Ardalan K, Gray EL, Lee J, Wolfe ML, Morgan GA, Pachman LM. Physical Function Trajectories in Children with Juvenile Myositis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/physical-function-trajectories-in-children-with-juvenile-myositis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/physical-function-trajectories-in-children-with-juvenile-myositis/