Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Date: Thursday, April 30, 2020
Title: Poster Session 1
Session Type: ACR Abstract Session
Session Time: 6:00PM-7:00PM
Background/Purpose: Radiological imaging is integral to the diagnosis of chronic nonbacterial osteomyelitis (CNO) and has been included as a central component in suggested diagnostic criteria [1,2]. Objectives of this study were: 1) to determine imaging modalities and features deemed important by radiologists in the diagnostic workup of suspected CNO cases; 2) to generate input from radiologists regarding monitoring of patients with CNO.
Methods: Population targeted were active attending radiologist physician members of the Society of Skeletal Radiology email list serve. The survey was administered online through RedCap. Descriptive statistics were conducted with continuous variables reported as medians/means and categorical variables as frequencies/percentages.
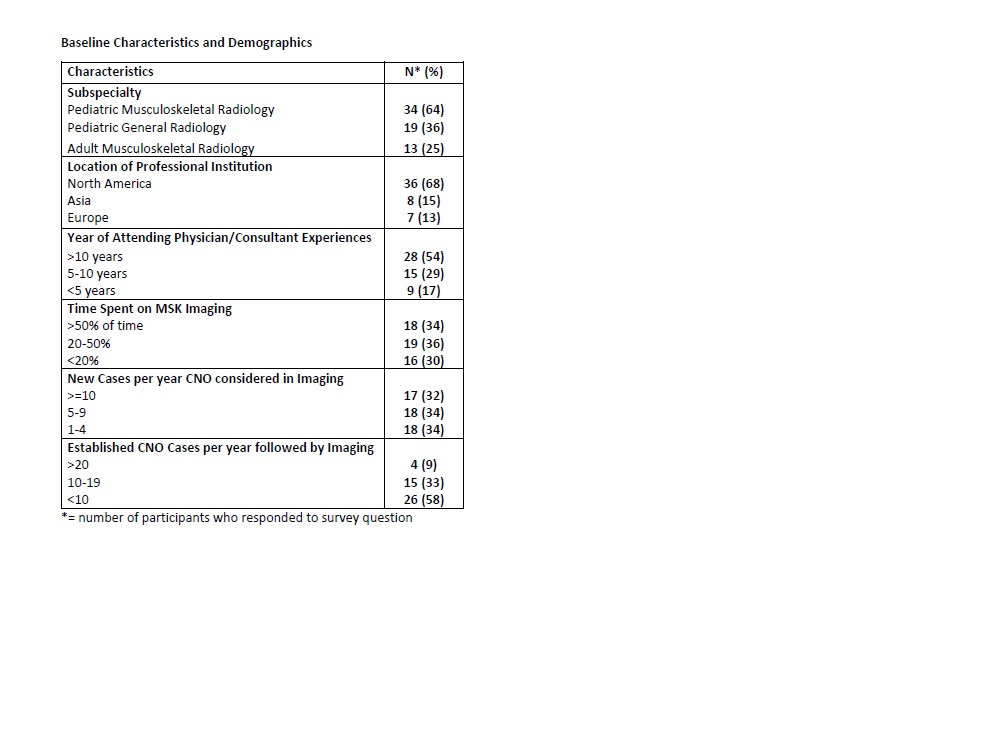
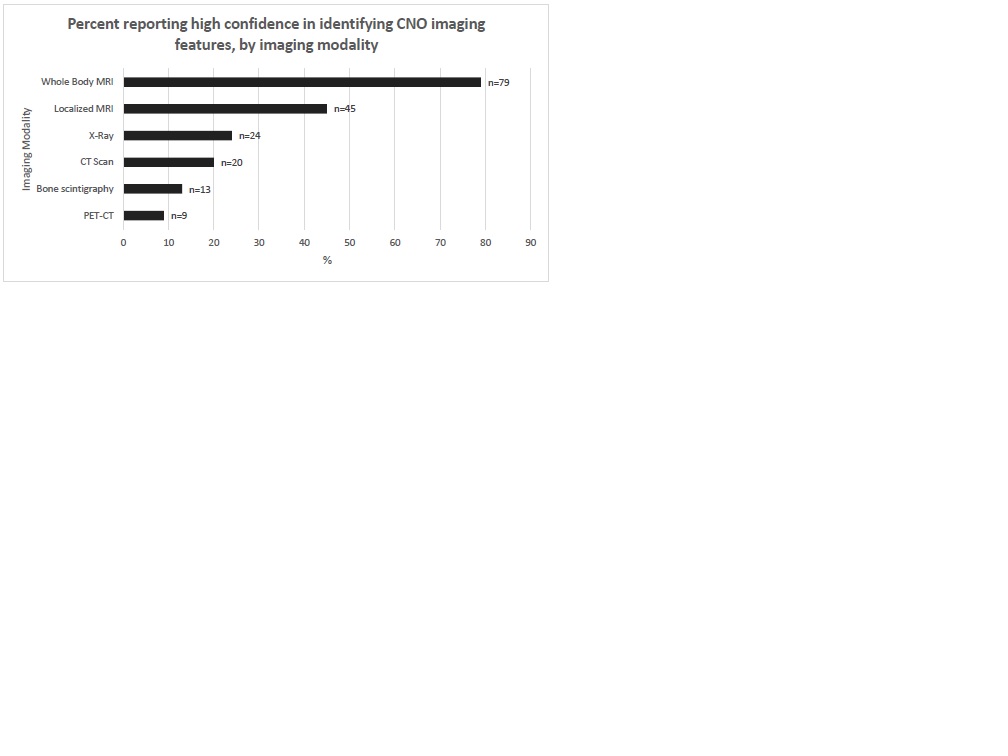
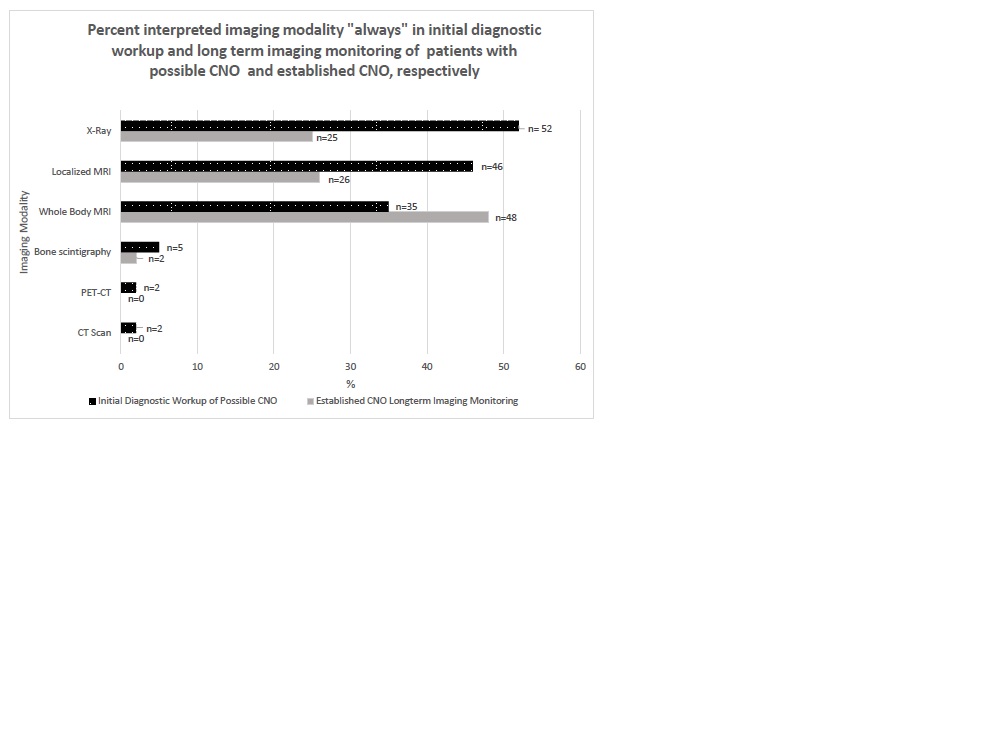
Results: A total of 66 respondents (5%) consented and completed the survey. The majority were pediatric radiologists, subspecializing in musculoskeletal radiology, with >10 years of experience (Table 1). Radiologists consider CNO in the radiological imaging interpretation differential diagnosis an average of 10 cases per year. 79% and 45% of respondents reported high confidence in identifying imaging features of CNO on whole body MRI (WBMRI) and localized MRI, respectively. The level of confidence drops to 24% and 13% when interpreting X-rays (XRs) and bone scintigraphy, respectively (Figure 1). Among all imaging modalities interpreted “always” in the initial diagnostic workup of potential cases of CNO, XRs (52%) were most commonly interpreted, followed by localized MRI (46%) and WBMRI (35%), which suggested the sequence of utilization of these three imaging modalities in new cases. In established cases of CNO, wherein WBMRI was the most frequently interpreted (48%), followed by localized MRI (26%) and XRs (25%) (Figure 2). Most common imaging features that led respondents to suggest a bone biopsy included disorganized bone formation (64%/56%), moth-eaten appearance (61%/56%), and lytic lesions (50%/44%) on XRs/CTs, respectively as well as the presence of soft tissue mass/swelling(68%/44%) and MRI signal hyperintensity of bone marrow at unifocal site (24%) on MRI. A majority of respondents preferred a combination of short tau inverse recovery (STIR), T1 and diffusion weighted imaging (DWI) sequences in the MRI images of potential CNO cases. 46% of respondents reported using an established WBMRI protocol at their institutions.
Conclusion: WBMRI is considered the most useful imaging modality for initial diagnosis and monitoring of CNO by radiologists. Certain morphological features including disorganized bone structure, moth-eaten appearance, lytic lesions, soft tissue mass/swelling and unifocal signal hyperintensity of bone marrow may result in increased chance of bone biopsy to exclude differential diagnoses. Findings from this survey will promote discussion within a focused group to develop imaging guidelines for the diagnostic workup and disease monitoring in CNO and contribute to earlier diagnosis and individualized care.
[1] Jansson, A et al. “Classification of nonbacterial osteitis.” Rheumatology (Oxford) 46, 1 (2007)
[2] Roderick, MR,et al. “Chronic recurrent multifocal osteomyelitis (CRMO).” Pediatric Rheumatology 14, 47 (2016)
To cite this abstract in AMA style:
Nuruzzaman F, Huang M, Hedrich C, Girschick H, Cherian J, Onel K, Sato T, Ferguson P, Zhao Y. Perspectives of Radiologist Physicians in the Imaging of Chronic Nonbacterial Osteomyelitis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/perspectives-of-radiologist-physicians-in-the-imaging-of-chronic-nonbacterial-osteomyelitis/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perspectives-of-radiologist-physicians-in-the-imaging-of-chronic-nonbacterial-osteomyelitis/