Session Information
Date: Sunday, November 12, 2023
Title: (0380–0422) RA – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Persisting pain with or without inflammation control is a common and debilitating symptom in rheumatoid arthritis (RA). Concerns have been raised that patients with non-inflammatory pain features might accumulate along the treatment path, but data is limited. The aim of this study was to examine prevalence and dynamics of unacceptable pain and unacceptable pain despite inflammation control (refractory pain), as well as predictors of these pain states, comparing TNF-inhibitor (TNFi) treatment lines in established RA.
Methods: RA patients starting a 1st, 2nd or ≥3rd TNFi treatment line 2004-2009 were identified in the South Swedish Arthritis Treatment Group register: N=993 for a 1st TNFi (77% women, mean age 58y, mean disease duration 10y); N=439 for a 2nd TNFi (83%, 56y, 14y); and N=143 for a ≥3rd TNFi (88%, 58y, 16y). A patient could contribute with data to more than one treatment line. Unacceptable pain was defined as >40 mm on a Visual Analogue Scale (VAS; 0-100 mm), according to the Patient Acceptable Symptom State (PASS),[1]and inflammation control captured through CRP < 10 mg/L combined with ≤1 swollen joint (of 28), as previously described.[2] Frequencies of unacceptable and refractory pain were respectively assessed at 0, 3, 6, 12 and 24 months and compared between treatment lines by Chi-2 test. Potential predictors at start of each TNFi line were estimated in relation to unacceptable/refractory pain at 24 months by logistic regression.
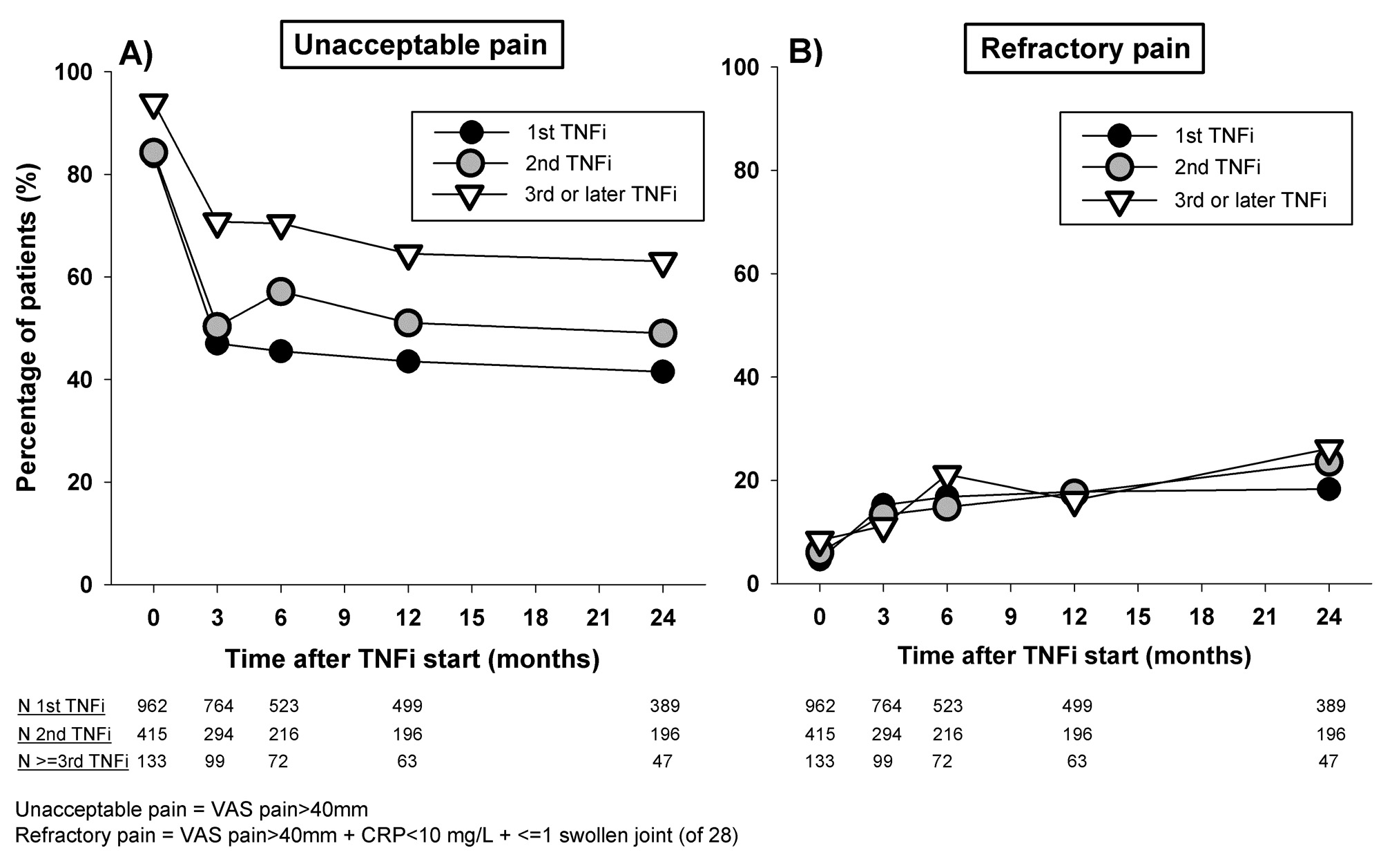
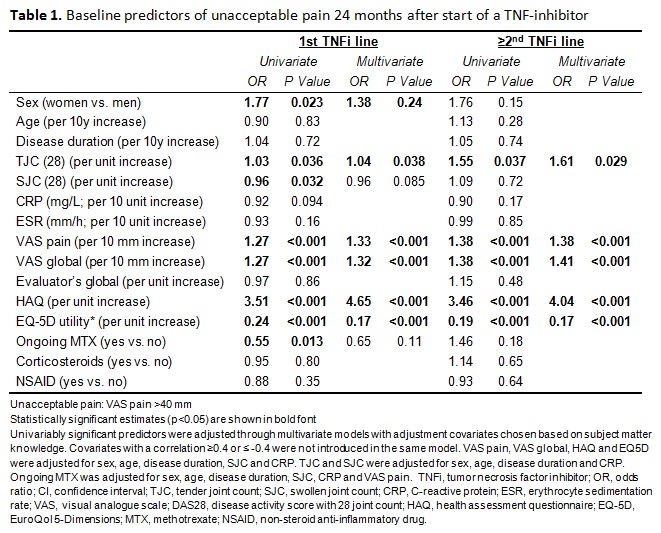
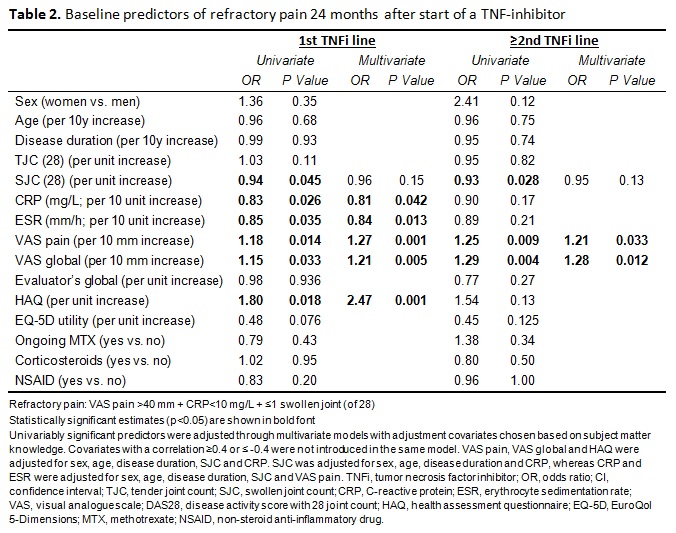
Results: In patients initiating a 1st TNFi, unacceptable pain decreased from 84% to 42% from therapy start to 24 months. Corresponding figures at 24 months were 49% for a 2nd TNFi (p=0.14 vs. 1st) and 63% for a ≥3rd TNFi (p=0.009 vs. 1st) (Figure). Refractory pain at 24 months was 18%, 24% and 26% for a 1st, 2nd and ≥3rd TNFi (2nd and ≥3rd line treatments non-significant vs. 1st line). Higher baseline HAQ and VAS pain/global, more tender joints, and lower EQ-5D utility were associated with a higher risk of 24-month unacceptable pain in patients starting both a 1st and later TNFi treatment lines, in adjusted analyses (Table 1). For refractory pain, higher VAS pain/global were the only significant predictors across treatment lines, while for a 1st TNFi refractory pain was also predicted by lower CRP and ESR, as well as higher HAQ (Table 2).
Conclusion: Unacceptable pain at 2 years follow-up is more frequent in later TNFi treatment lines and almost half of this pain load is due to pain indicative of a non-inflammatory mechanism. Predictors of unacceptable pain are largely stable across treatment lines, while for refractory pain they vary with line of treatment. The results suggest a selection of RA patients with intense pain, including non-inflammatory components, in later TNFi treatment lines. This highlights a need for additional pharmacologic and non-pharmacologic therapies that more specifically target various pain features.
1. Tubach et al. ArthritisCareRes 2012;64:1699-707
2. Olofsson et al. Arthritis Care Res 2021;73:1312-21
To cite this abstract in AMA style:
Roseman C, Karlsson Wallman J, Einarsson J, Mogard E, Lindqvist E, Kapetanovic M, Olofsson T. Persistent Pain and Its Predictors After Start of Anti-TNF Therapy in Rheumatoid Arthritis – Is Line of Treatment Linked to Different Pain Patterns? [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/persistent-pain-and-its-predictors-after-start-of-anti-tnf-therapy-in-rheumatoid-arthritis-is-line-of-treatment-linked-to-different-pain-patterns/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/persistent-pain-and-its-predictors-after-start-of-anti-tnf-therapy-in-rheumatoid-arthritis-is-line-of-treatment-linked-to-different-pain-patterns/