Session Information
Date: Monday, November 14, 2022
Title: Metabolic and Crystal Arthropathies – Basic and Clinical Science Poster
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Peripheral vascular disease (PVD) causes substantial morbidity and mortality. Patients with gout are known to have increased coronary artery disease risk but less is known about their risk for PVD. Using electronic medical record data from the national Veterans Health Administration (VHA) system, we examined associations between gout, PVD and PVD sequelae including lower extremity amputation (LEA). We used diabetes (DM), a well-established risk factor for PVD, as a positive comparator.
Methods: We collected deidentified data from all VHA patients nationally with an active medical record from 2014–2018. After identifying PVD prevalence among all patients, we selected a random sample of 20% for initial analysis to allow for later internal validation. We classified gout, DM, and PVD using ICD-10 diagnosis codes. CPT codes were used to identify amputations as a surrogate for severe PVD. Using a multinomial logistic regression approach, we modeled odds of PVD and LEA in our 20% sample cohort as functions of gout, DM, and characteristics including race, ethnicity, sex, age, region, BMI, serum urate (SU) and baseline creatinine.
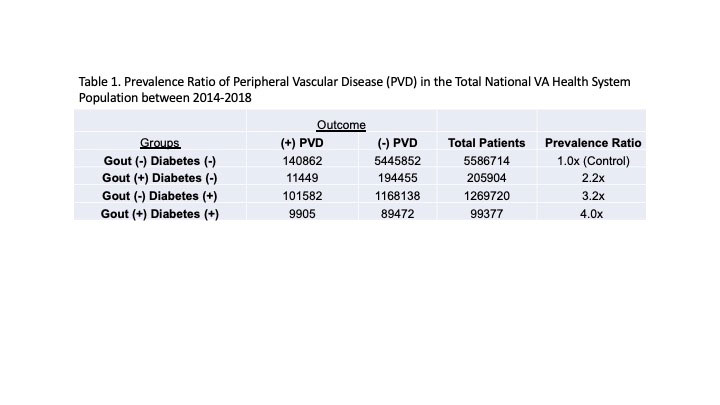
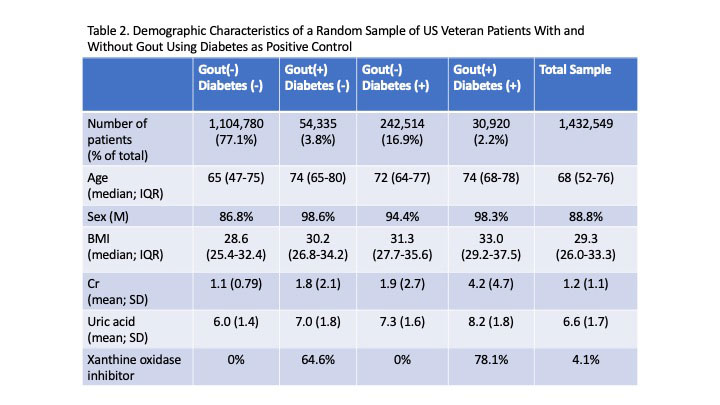
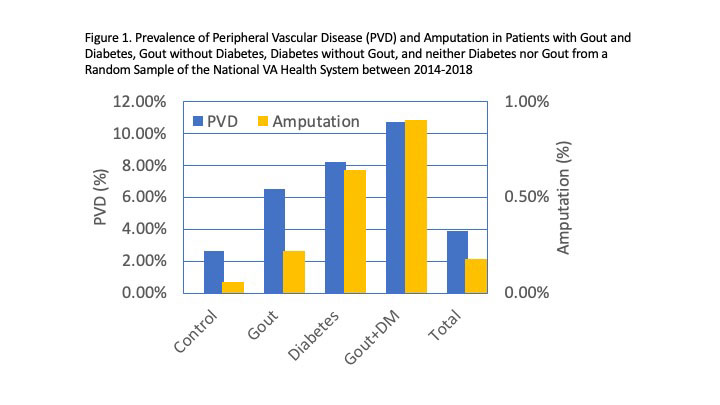
Results: 7,161,715 records were reviewed. In the total population, PVD identified through diagnosis code was 2.2x more prevalent in those with gout alone, 3.2x more prevalent in those with DM without gout, and 4x more prevalent in those with gout+DM, than those with neither (controls) (Table 1). Amputations by CPT codes yielded similar findings: 2.5x more prevalent in gout alone, 4.2x in DM without gout, and 5.8x in gout+DM compared with controls. Among the 20% randomly sampled population, controls tended to be younger (median 65, IQR 47–75 years) with lower BMI (median 29, IQR 25–32 years), while those with gout+DM tended to be older (median 74, IQR 68–78 years) with higher BMI (median 33, IQR 29–37) than patients with either gout or DM alone (Table 2). Patients with gout+DM had the highest mean SU at 8.2 mg/dL (SD 1.8) compared to 7.3 (SD 1.6) in DM only, 7.0 (SD 1.8) in gout only and 6.0 (SD 1.4) in controls. Patients with gout alone had rates of amputations that were higher than controls (consistent with a prior report1), but lower than those with DM alone (Figure 1). Patients with gout+DM had the highest rates of amputations. After controlling for potential risk factors, those with gout were 1.7x (CI:1.68-1.82) more likely to have PVD. Patients with DM were 2.6x (CI: 2.53-2.63) more likely. Patients with gout+DM were 3.2x (CI: 3.0-3.4) more likely to have PVD.
Conclusion: In a national VA cohort, individuals with gout were at significantly greater risk for PVD and LEA than patients without gout, but at lesser risk than individuals with DM, even after adjustment for confounders. Individuals with gout+DM were at the highest risk for PVD and LEA, although the interaction did not appear to be synergistic. These data suggest that gout is an underrecognized risk factor for PVD and indicate the importance of assessing for PVD when caring for gout patients.
1Mikuls TR et al. Comparison of Rates of Lower Extremity Amputation in Patients With and Without Gout in the US Department of Veterans Affairs Health System. JAMA Netw Open. 2022;5(1):e2142347.
To cite this abstract in AMA style:
Leung N, Toprover M, Fang C, Pillinger M, Pendse J. Peripheral Vascular Disease and Sequelae in Individuals with Gout, Diabetes, or Both Among US Veterans [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/peripheral-vascular-disease-and-sequelae-in-individuals-with-gout-diabetes-or-both-among-us-veterans/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/peripheral-vascular-disease-and-sequelae-in-individuals-with-gout-diabetes-or-both-among-us-veterans/