Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Pericoronary adipose tissue attenuation (PCATa) reflects the composition of the fat directly surrounding the coronary arteries and is associated with coronary wall inflammation. In general patients with coronary atherosclerosis, PCATa, particularly around the right coronary artery (RCA), predicted plaque burden, plaque vulnerability, and optimized cardiovascular risk estimates. The volume of epicardial adipose tissue (EATv) contained between the free cardiac surface and the visceral pericardium, which includes PCAT, was linked to coronary atherosclerosis burden and progression in rheumatoid arthritis (RA). We here explore differences in PCATa and PCATa-atherosclerosis associations between RA and controls and whether PCATa relates to coronary plaque burden and composition independently of EATv in RA.
Methods: PCATa around the proximal left anterior descending (LAD), left circumflex (LCx) and RCA, total EATv, and atherosclerosis burden and composition (noncalcified, mixed and calcified) were evaluated with coronary computed tomography angiography (CCTA) in 150 RA patients and 120 age and gender-matched controls without known coronary artery disease. Linear regression evaluated the association between RA and PCATa. Negative binomial regression explored the association of collective (3-artery) and artery-specific PCATa on numbers of plaques (total and plaque subtypes). RA x PCATa interactions evaluated the moderating effect of disease state on plaque outcomes.
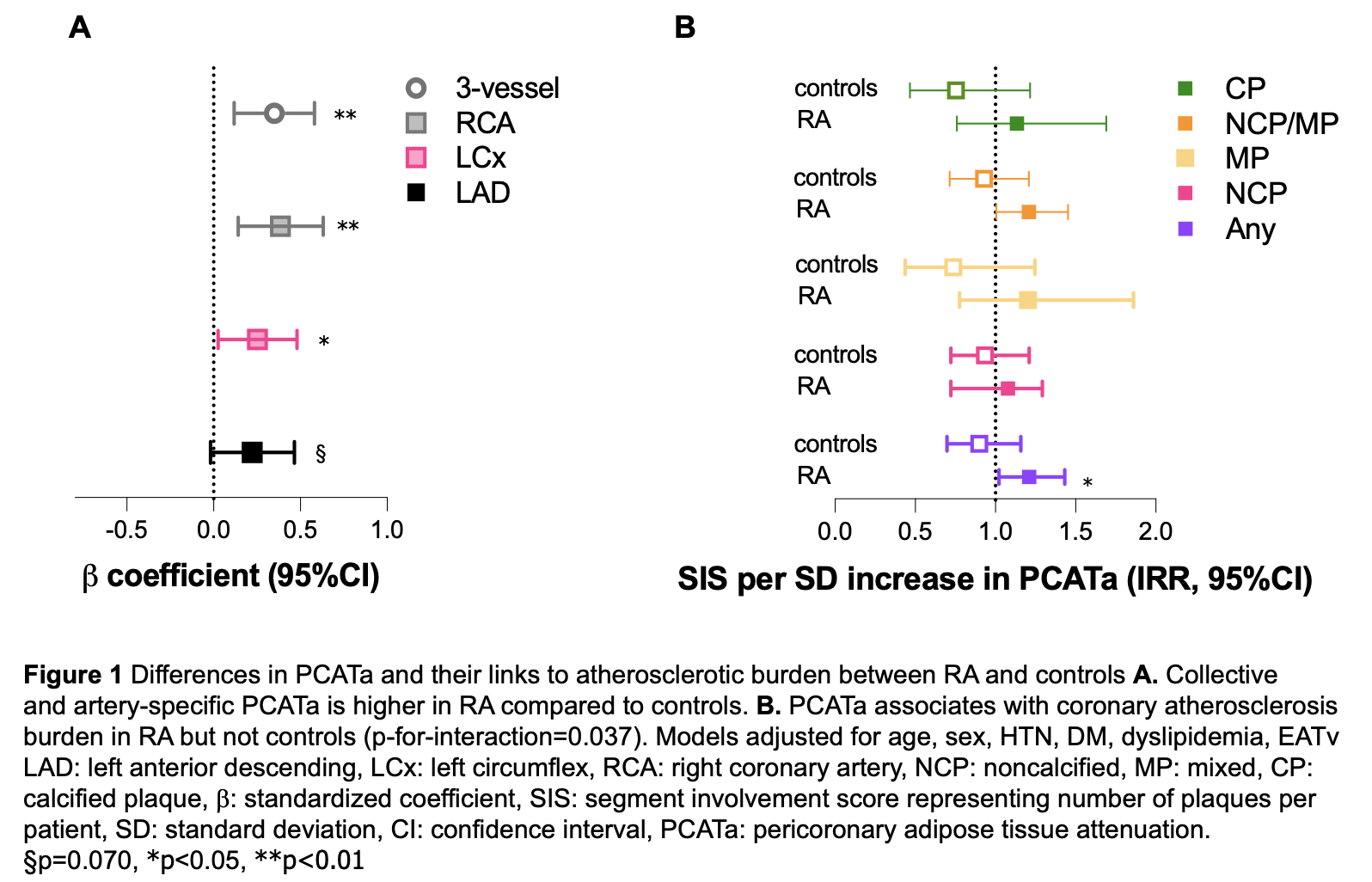
Results: Collective PCATa (standardized b-coefficient 0.35, 95% confidence interval 0.12-0.58) and artery-specific PCATa around LCx (b 0.25, 95%CI 0.03-0.48) and RCA (b 0.39, 95%CI 0.14-0.63) was higher in RA compared to controls (Figure 1A) after adjustments for age, sex, hypertension, diabetes, dyslipidemia and EATv. Collective PCATa (per standard deviation increase) associated with 21% more total plaques in RA (incidence rate ratio-IRR 1.21, 95%CI 1.02-1.43) but not in controls (p for interaction=0.037, Figure 1B) after similar adjustments. In patients with RA, collective PCATa (IRR 1.23, 95%CI 1.03-1.48) and artery-specific PCATa around LCx (IRR 1.20, 95%CI 1.01-1.44) and RCA (IRR 1.19, 95%CI 1.00-1.41) associated with more plaques, especially those with soft components (noncalcified or mixed, Figure 2A and B) after adjustment for atherosclerotic cardiovascular risk score, EATv, erythrocyte sedimentation rate, prednisone, and statin use. There was no difference in artery-specific PCATa among matched normal arteries in RA patients with and without atherosclerosis (all p >0.05). In contrast, upon comparing matched arteries with vs. without plaque, PCATa was higher only around atherosclerotic LCx vessels.
Conclusion: Cumulative PCATa is higher and is linked to coronary atherosclerosis burden in RA but not controls. Cumulative and artery-specific PCATa in RA is linked to more total, soft, and vulnerable plaques, and provides additional information over EATv on atherosclerosis burden. The nature of compositional changes in PCAT may vary regionally and reflect the presence of explicit structural changes, such as plaque, in the underlying vessel wall.
To cite this abstract in AMA style:
Enevoldsen F, Ormseth S, Masic D, Budoff M, Hauge E, Karpouzas G. Pericoronary fat enhancement in rheumatoid arthritis differs from controls and associates with coronary atherosclerosis independently of epicardial fat volume [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/pericoronary-fat-enhancement-in-rheumatoid-arthritis-differs-from-controls-and-associates-with-coronary-atherosclerosis-independently-of-epicardial-fat-volume/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pericoronary-fat-enhancement-in-rheumatoid-arthritis-differs-from-controls-and-associates-with-coronary-atherosclerosis-independently-of-epicardial-fat-volume/

.jpg)