Session Information
Session Type: Abstract Submissions
Session Time: 5:30PM-7:00PM
Background/Purpose:
Patients with childhood-onset SLE (cSLE) have a higher incidence of renal disease and may receive more intensive immunosuppression as compared to individuals with adult-onset SLE (aSLE). Growth failure, a proposed measure of damage in cSLE, may be associated with disease activity and steroid use. The goal of our study was to compare final height to expected height in adults with cSLE vs. aSLE.
Methods:
Data derive from telephone or online surveys from the 2002-07 cycles of the Lupus Outcomes Study (LOS) and the 2012-16 cycles of the Pediatric Lupus Outcomes Study (PLOS), two cohorts of adult SLE patients. SLE diagnosis was confirmed by chart review using the ACR SLE classification criteria. Participants diagnosed at age < 18 years were defined as cSLE (n=152). Respondents reported their height and both parentsÕ heights; participants with complete height data (n=648) were included in this analysis. Expected adult height was estimated from mid-parental height using the Tanner formula, a validated measure. Multivariate linear regression was used to compare the difference between expected and final height for cSLE and aSLE participants, adjusting for gender and ethnicity.
Results:
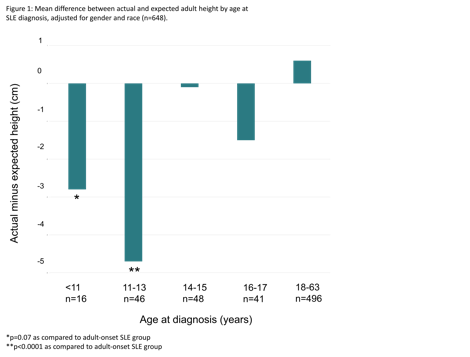
Participants with cSLE were younger (mean age 27±9 vs. 49±9 years; p<0.0001), more likely to be male (12% vs 6%; p=0.01) and less likely to be white (52% vs. 70%; p<0.0001). Mean age at diagnosis was 14±3 vs. 33±10 years (p<0.0001). Respondents with cSLE were more likely to have ever required dialysis (12% vs 7%; p=0.06). Nearly all cSLE participants reported a history of steroid use (99% vs. 94%; p=0.02) and were also more likely to have been exposed to cyclophosphamide (22% vs. 13%; p=0.001). Participants with cSLE were on average 1.4 cm shorter than expected before adjustment, and 2.1 cm shorter than expected after controlling for gender and ethnicity (95% CI -3.3, -1.0). This differed significantly from aSLE participants (p=0.0005), who were 0.6 cm taller than expected (95% CI 0.06, 1.1). Participants diagnosed at age 11-13 years showed the greatest difference between actual and expected height (Figure 1). This group was shorter than expected by 4.7 cm after adjustment (95% CI -6.5, -2.8), which differed significantly from the aSLE group (p<0.0001). Those diagnosed prior to age 11 years (n=16) were 2.8 cm shorter than expected after adjustment (95% CI -5.9, 0.3), which approached significance when compared with aSLE group (p=0.07).
Conclusion:
Onset of SLE in childhood appears to be associated with shorter than expected adult stature. Onset of SLE in the peri-pubertal period, a time of rapid linear growth, may have a particularly significant impact on final adult height. Further studies are needed to delineate the relative contributions of disease- and treatment-related risk factors, such as chronic inflammation, renal insufficiency and chronic steroid use, to shorter-than-expected adult height in cSLE.
To cite this abstract in AMA style:
Heshin-Bekenstein M, Hersh AO, von Scheven E, Lawson E. Peri-pubertal Onset of Systemic Lupus Erythematosus is Associated with Shorter than Expected Adult Height [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 4). https://acrabstracts.org/abstract/peri-pubertal-onset-of-systemic-lupus-erythematosus-is-associated-with-shorter-than-expected-adult-height/. Accessed .« Back to 2017 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/peri-pubertal-onset-of-systemic-lupus-erythematosus-is-associated-with-shorter-than-expected-adult-height/