Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Causes and risk factors for variations in SLE disease activity and symptom severity are incompletely understood. Prior studies suggest a link between stressful life events (e.g. trauma), perceived stress, and greater disease severity. We examined whether (1) high levels of stress during the COVID-19 pandemic—both generalized and attributed to COVID-19—were associated with worse patient-reported outcomes (PROs) among patients with lupus, and (2) increases in perceived stress concurrent with the pandemic associated with increases in symptoms and/or incident SLE flares.
Methods: Participants, drawn from the California Lupus Epidemiology Study (CLUES), were ≥18 years old and met ACR criteria for SLE. Data derive from interviews conducted during the COVID-19 pandemic and study assessments during the prior year. General stress was measured using the 4-item Perceived Stress Scale (PSS, range 0-16). Scores in the top quartile were categorized as high stress. High stress from COVID-19 was assessed by asking whether it had caused “a great deal of stress or worry” and/or “the most stressful situation I have been through”. PROs included: self-report disease activity (SLE Activity Questionnaire, SLAQ), pain severity (scale 1-10), fatigue (PROMIS fatigue scale), cognitive function (PROMIS cognitive ability scale), and self-report SLE flares (prior month). Multivariable linear and logistic regression first evaluated associations of generalized and COVID-19-specific stress with PROs during the pandemic while controlling for potential confounders (age, sex, race, education, income, smoking, disease duration, and disease damage), and then modeled changes in PROs from pre-pandemic to during the pandemic as a function of change in perceived stress (by PSS). We calculated adjusted means for each outcome based on the multivariable regression.
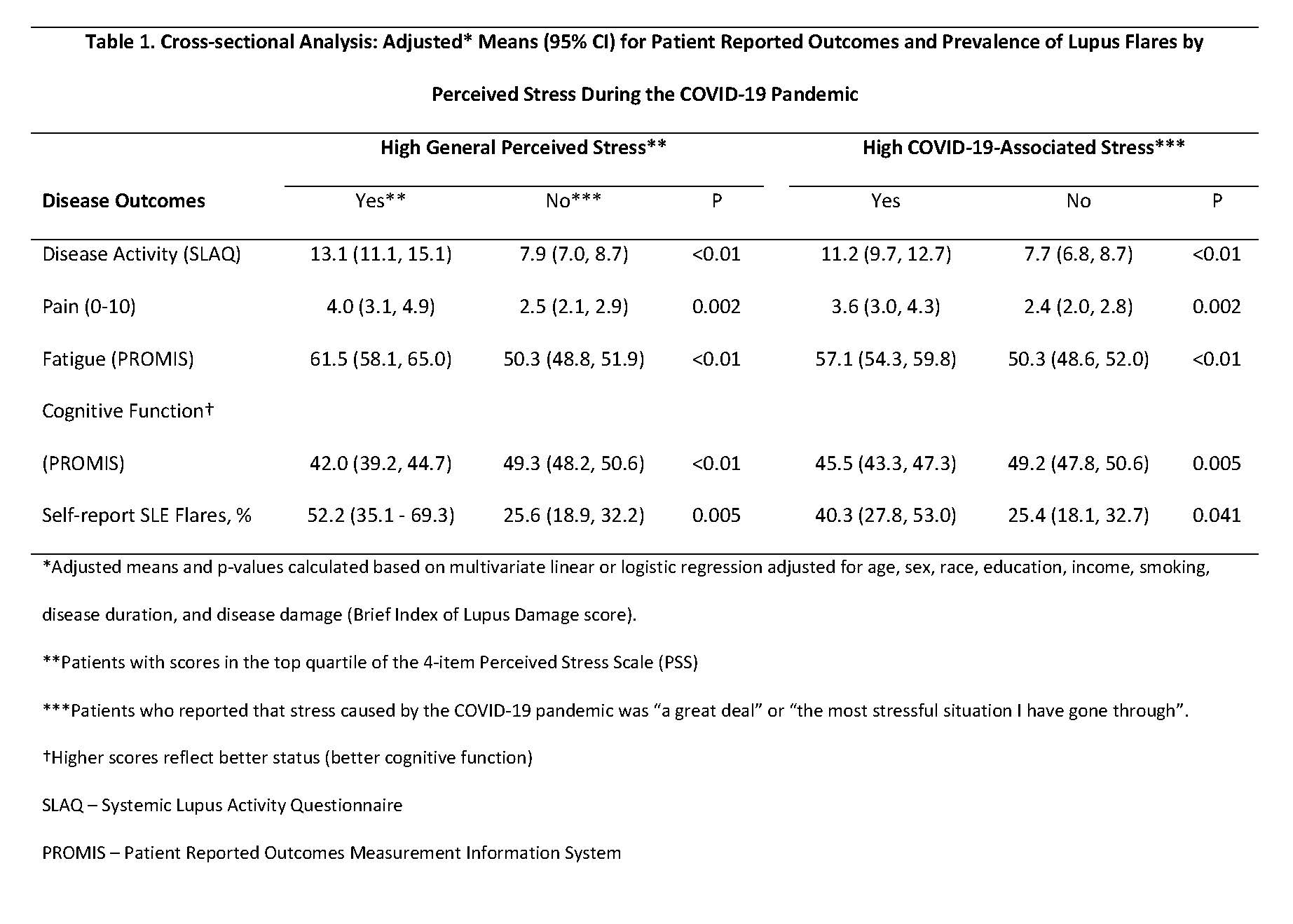
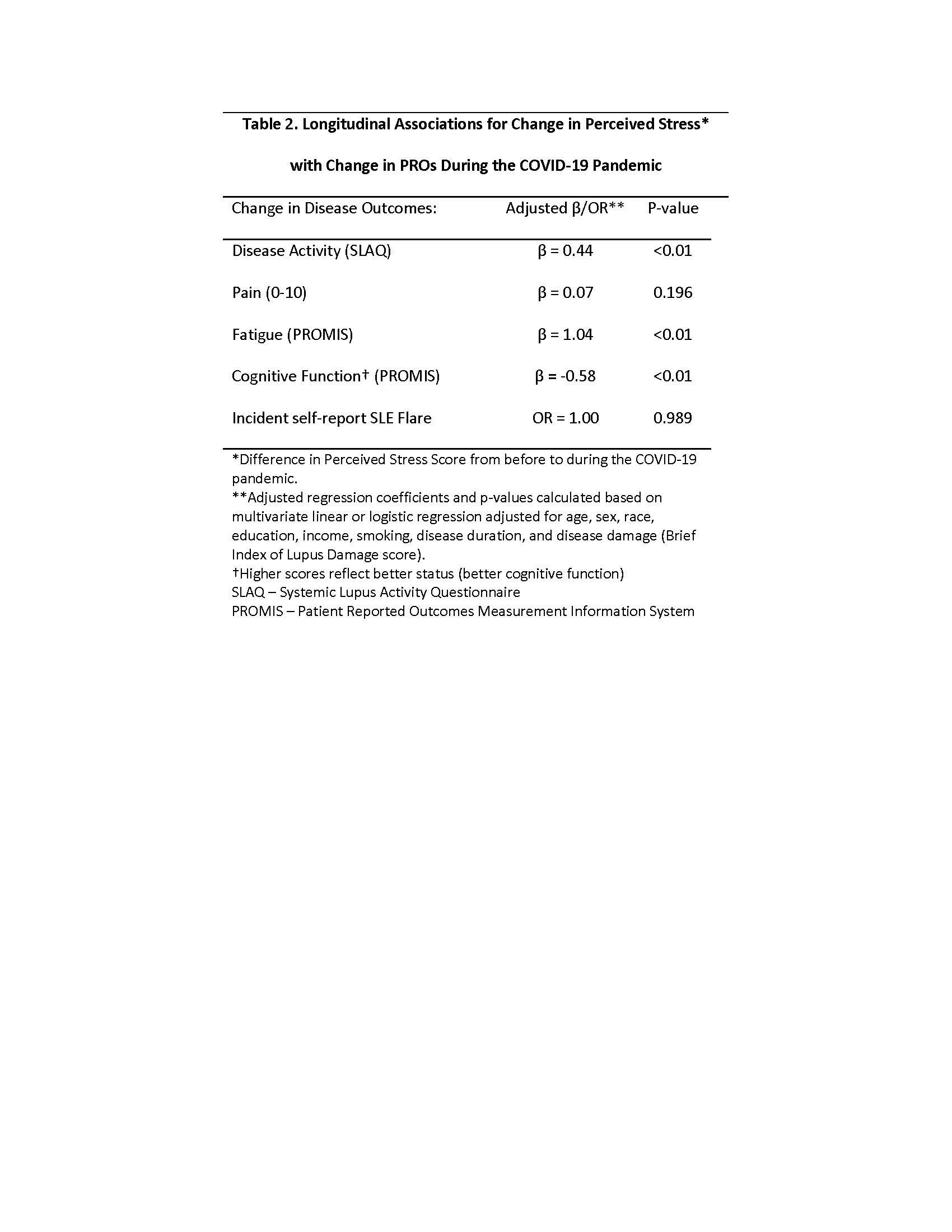
Results: The sample (n=201) was 91% female; 36% white, 27% Asian, 24% Hispanic, and 9% African American; mean age 50 (± 14) years; 17% with poverty-level income; and mean disease duration 22 (± 10) years. During the COVID-19 pandemic, 29% reported severe stress related to the health crisis. The mean PSS score in the high stress group was 10.1 (± 1.4), compared with 4.4 (± 2.6) among the rest of the cohort. In the cross-sectional multivariate regression model, high stress by both measures (PSS and COVID-19 stress question) was associated with worse scores for each PRO: greater self-reported disease activity, more pain, more fatigue, lower cognitive function, and higher frequency of flares (Table 1). In the longitudinal analysis, increase in stress independently associated with an increase in disease activity, increase in fatigue, and decrease in cognitive function, but no significant change in pain severity or flares (Table 2).
Conclusion: In a racially diverse SLE cohort, psychological stress during the COVID-19 pandemic independently associated with worse PROs including self-reported disease activity, fatigue, and cognitive dysfunction. Evidence-based non-pharmacologic interventions to bolster stress resiliency are urgently needed to improve outcomes in this patient population during the ongoing health crisis.
To cite this abstract in AMA style:
Patterson S, Trupin L, DeQuattro K, Lanata C, Dall'Era M, Yazdany J, Katz P. Perceived Stress During the COVID-19 Pandemic Independently Associates with Worse Patient-Reported Outcomes in Systemic Lupus Erythematosus (SLE) [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/perceived-stress-during-the-covid-19-pandemic-independently-associates-with-worse-patient-reported-outcomes-in-systemic-lupus-erythematosus-sle/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perceived-stress-during-the-covid-19-pandemic-independently-associates-with-worse-patient-reported-outcomes-in-systemic-lupus-erythematosus-sle/