Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Pediatric rheumatologists are facing a shortfall of providers and in multiple states, patients do not have readily accessible care for rheumatologic issues. Our clinic noticed an increase in pediatric rheumatology referrals over the past two years with subsequent increase in wait times to be seen in clinic. We sought to evaluate our referrals to ensure that referrals were appropriate to be seen in the rheumatology clinic or be directed to another specialty, escalate referrals for certain diagnoses that required immediate care, and to ensure that we had adequate records prior to clinic appointments to aid in patient care and patient satisfaction.
Methods: Our team centralized all referrals to a database where referrals were reviewed by a pediatric rheumatologist from March 2023 to March 2024. If records were not sent with the referral, the referring provider was contacted for pertinent records. The referral was then assessed for appropriateness for the rheumatology clinic as well as the timeframe that the patient should be seen. Patients felt to have potential diagnoses concerning for the following were escalated with clinic staff scheduling these patients with the goal of being seen in the pediatric rheumatology in one week: systemic lupus erythematosus, juvenile dermatomyositis, systemic juvenile idiopathic arthritis, systemic vasculitis, and chronic recurrent multifocal osteomyelitis. If the referral was felt appropriate and did not need to be escalated, the referral was sent to our contact center to schedule first available.
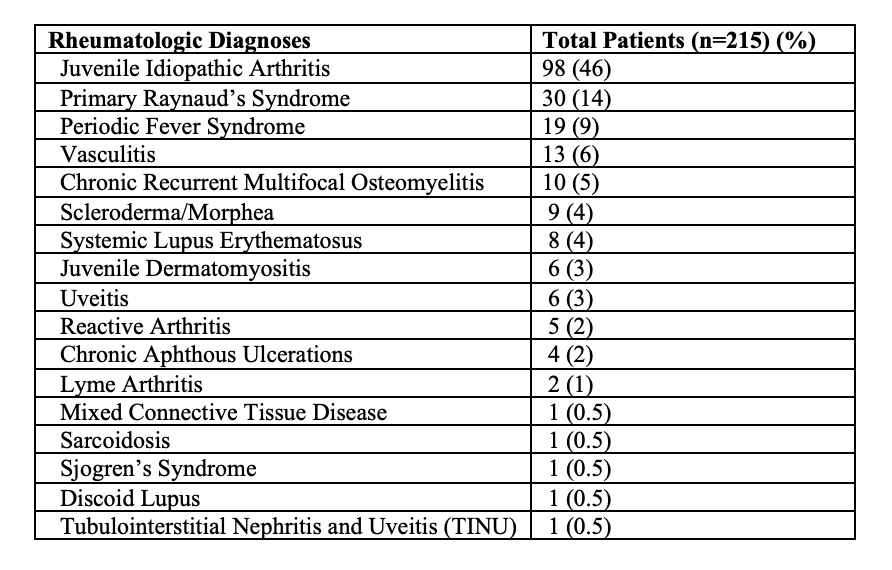
Results: During this one-year time frame, we received 1,642 referrals to the pediatric rheumatology clinic with 1092 (67%) being female. Of those, 86 (5.2%) were felt to be inappropriate for the rheumatology clinic. Our institution was unable to reach 229 (13.9%) families to schedule their appointments and of those scheduled, 70 (4.3%) did not keep their appointment and 13 (0.8%) had yet to have their appointment in clinic. Of the 1,238 patients seen during that time, only 215 patients (17%) were diagnosed with a rheumatic condition (Table 1) with 69 (5.6%) patients being monitored at future appointments for evolution of their symptoms. Most patients that were not felt to have a rheumatologic diagnosis were diagnosed with amplified pain, hypermobility/Ehlers-Danlos syndrome, combination of amplified pain and hypermobility, or a positive antinuclear antibody. Wait times for clinic decreased from the beginning of March 2023 where 25.6% of patients were seen within 14 days to 53.7% of patients being seen within 14 days by the first week of April 2024.
Conclusion: To streamline our referral process to improve access, schedule patients with critical diagnoses in clinic in a timely manner, as well as to ensure that patients seen in clinic were appropriate for rheumatology, we evaluated our referral pattern for a 12-month time span. Most referrals seen in the clinic were diagnosed with a non-rheumatic condition with only 17% of patients felt to have a rheumatologic diagnosis. Future work should include additional education for referring practitioners including appropriate lab testing and clinic referrals to reduce the burden for a small work force and save healthcare dollars.
To cite this abstract in AMA style:
Fox E, Quinn S, Lytch A, Williams A, Harris J, Cooper A. Pediatric Rheumatology Clinic Referral Patterns at a Large Midwestern Center [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/pediatric-rheumatology-clinic-referral-patterns-at-a-large-midwestern-center/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pediatric-rheumatology-clinic-referral-patterns-at-a-large-midwestern-center/