Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) constitutes one of the main causes of mortality in patients with autoimmune diseases (ADs) [1]. The early diagnosis of AD-ILD+ is sometimes a challenge due to the similarity of the clinical, pathological, and epidemiological features with idiopathic pulmonary fibrosis (IPF) [1]. Given the differences in long-term prognosis and treatments in these diseases, establishing a precise biomarker is crucial for changing the diagnosis of IPF to AD-ILD, or from one AD to another AD [1,2]. In this sense, transforming growth factor-β (TGF-β) and platelet-derived growth factor (PDGF) are the major profibrogenic agents and they have been involved in different lung pathologic conditions [3,4].
Accordingly, this work aimed to study the expression of PDGFA and TGFB1 in AD-ILD+ as potential biomarkers for the precise diagnosis of the disease.
Methods: Peripheral blood was collected from a total of 112 AD-ILD+ patients: patients with rheumatoid arthritis (RA)‐ILD+ (n=39), systemic sclerosis (SSc)‐ILD+ (n=36), inflammatory myopathies (IM)-ILD+ (n=30) and Sjögren’s syndrome (SS)-ILD+ (n=7); as well as from 146 IPF patients. The relative PDGFA and TGFB1 mRNA expression was quantified by qPCR.
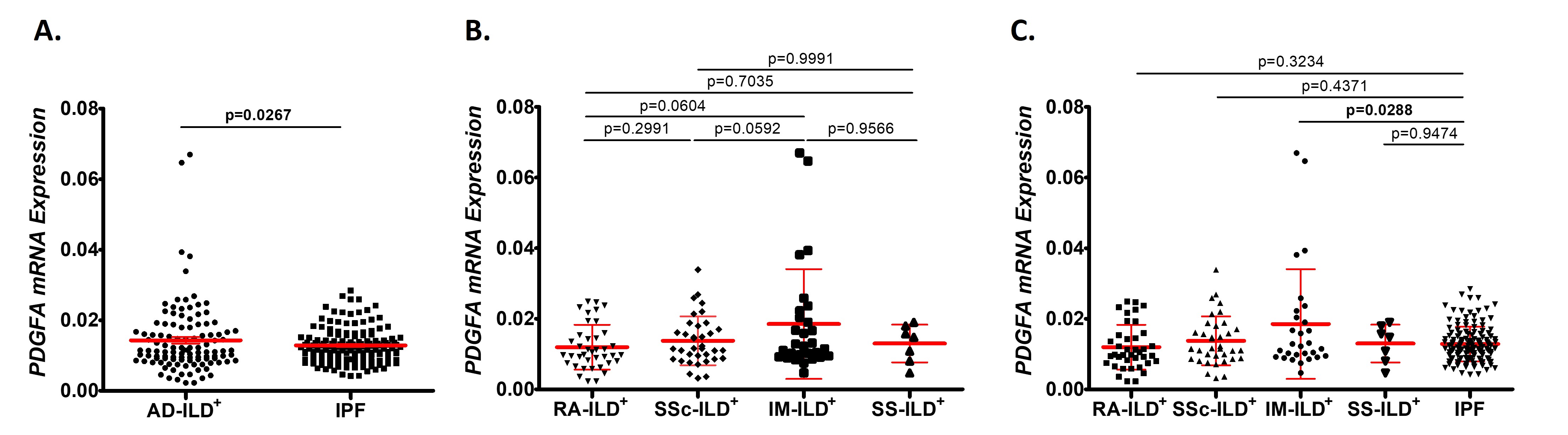
Results: Regarding PDGFA, a higher expression was found in AD-ILD+ patients compared to those with IPF (p=0.0267, Figure 1A). When the whole cohort of AD-ILD+ patients was stratified by underlying AD, patients with IM-ILD+ showed higher PDGFA expression than IPF patients (p=0.0288, Figure 1C). However, no differences in PDGFA expression were found between the types of underlying AD in AD-ILD+ patients (Figure 1B).
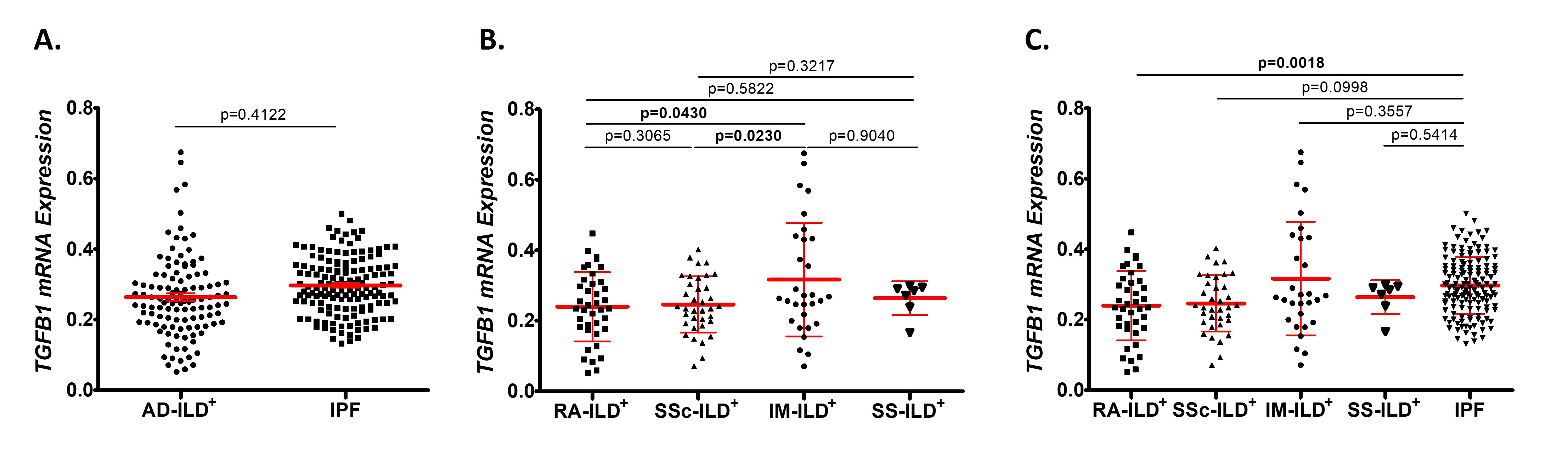
Concerning TGFB1, RA-ILD+ patients presented a lower expression compared to IPF patients (p=0.0018, Figure 2C), although this difference was not represented when the whole cohort of AD-ILD+ patients was compared with IPF patients (Figure 2A). Furthermore, when TGFB1 expression was compared between patients with AD-ILD+ stratified by underlying AD, IM-ILD+ patients showed the highest expression of TGFB1, although this difference was significant with RA-ILD+ and SSc-ILD+ patients (p=0.0430 and p=0.0230, respectively, Figure 2B).
The ability of PDGFA and TGFB1 to discriminate IM-ILD+ and RA-ILD+ patients from IPF patients, respectively, was further evaluated by ROC curves (Figure 3A and B, respectively). Interestingly, we found that TGFB1 was useful for differential diagnosis between RA-ILD+ and IPF (p=0.0017, Figure 3B).
Additionally, patients with AD-ILD+ exhibited a relationship between PDGFA mRNA expression and TGFB1 mRNA expression (r=0.7092, p< 0.0001). However, no significant correlation was found between PDGFA and TGFB1 expression and clinical features in AD-ILD+ patients.
Conclusion: Our findings showed the potential usefulness of the TGFB1 expression evaluation as a complementary tool for the differential diagnosis between patients with RA-ILD+ and IPF.
References:[1] Respirology.2016;21(2):245-58; [2] Respir Investig.2024;62(3):465-480; [3] J Exp Med. 2020;217(3):e20190103; [4] Life(Basel).2022;12(5):658.
Research funded by IDIVAL funds (NVAL23/02). Personal funds, JCB-L:FI22/00020(ISCIII-ESF); RL-M:CPII21/00004(ISCIII-ESF)
To cite this abstract in AMA style:
Pulito-Cueto V, Atienza-Mateo B, Iturbe-Fernández D, Mora-Cuesta V, Batista-Liz J, Sebastián Mora-Gil M, Cifrián J, Blanco-Alonso R, Lopez-mejias R. PDGFA and TGFB1, Key Genes to Discriminate Autoimmune Diseases-Related Interstitial Lung Disease from Idiopathic Pulmonary Fibrosis? [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/pdgfa-and-tgfb1-key-genes-to-discriminate-autoimmune-diseases-related-interstitial-lung-disease-from-idiopathic-pulmonary-fibrosis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pdgfa-and-tgfb1-key-genes-to-discriminate-autoimmune-diseases-related-interstitial-lung-disease-from-idiopathic-pulmonary-fibrosis/