Session Information
Date: Tuesday, October 28, 2025
Title: (2052–2078) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Comorbidities contribute to the disease burden in idiopathic inflammatory myopathies (IIMs). Understanding their distribution and predictors across IIM subtypes can guide tailored strategies. This study aimed to evaluate the patterns of comorbidities across IIM subsets, identify predictors of physical and mental comorbidities, and characterize comorbidity clusters.
Methods: This cross-sectional study used data from the Collating the Voices of Patients with Autoimmune Diseases study. Adults with specialist-diagnosed, self-reported IIMs were included. The validated Functional Comorbidities Index (FCI) was used to collect information on comorbidities. Subgroup comparisons were conducted across IIM subtypes. Descriptive statistics were performed and binary logistic regression was used to identify predictors of mental and physical health comorbidities. Hierarchical cluster analysis was applied to derive composite comorbidity clusters using R.
Results: Of 14,902 respondents, 1,209 IIM patients (69.6% female) were included [Fig.1A, 1B], with a median age and disease duration of 60 and 17 years, respectively (Table 1). The most common comorbidities were mental health conditions (32.1%), cardiovascular diseases (32.0%), and musculoskeletal disorders (23.3%). Mental (41.4%) and musculoskeletal (45.2%) comorbidities were most common in overlap myositis (OM). Cardiovascular conditions were most common in inclusion body myositis (IBM) (45.2%) [Fig.1C]. Predictors of mental health comorbidities included older age (OR:0.98; 95%CI=0.96-0.99), high Human Development Index (HDI) (OR:4.35; 95%CI=1.72-1.75), and alcohol intake (2-4 times/month) (OR:0.44; 95%CI=0.24-0.79). Predictors of physical health comorbidities were older age (OR:1.05; 95%CI=1.02-1.07), high HDI (OR:5.32; 95%CI=1.26-22.39), alcohol intake (2-4 times/month) (OR:0.45; 95%CI=0.23-0.90), and disease damage (OR:1.13; 95%CI=1.01-1.26). Hierarchical cluster analysis identified 3 comorbidity clusters. Cluster 1 was characterized by Hispanic ethnicity, lower HDI, and low multimorbidity, with notable immune-mediated necrotizing myopathies representation but limited variance. Cluster 2 was male-dominated, had very high HDI and moderate mental and physical comorbidity levels, and included the highest proportion of IBM and polymyositis. Cluster 3 showed the highest multimorbidity burden, dominated by dermatomyositis and anti-synthetase syndrome.
Conclusion: Comorbidities vary across IIM subtypes. Older age and high HDI predict both mental and physical health comorbidities, while higher disease damage predicts physical health comorbidity. Comorbidity clusters reveal distinct IIM subtype distributions, highlighting subtype-specific comorbidity patterns that may guide personalized clinical management.
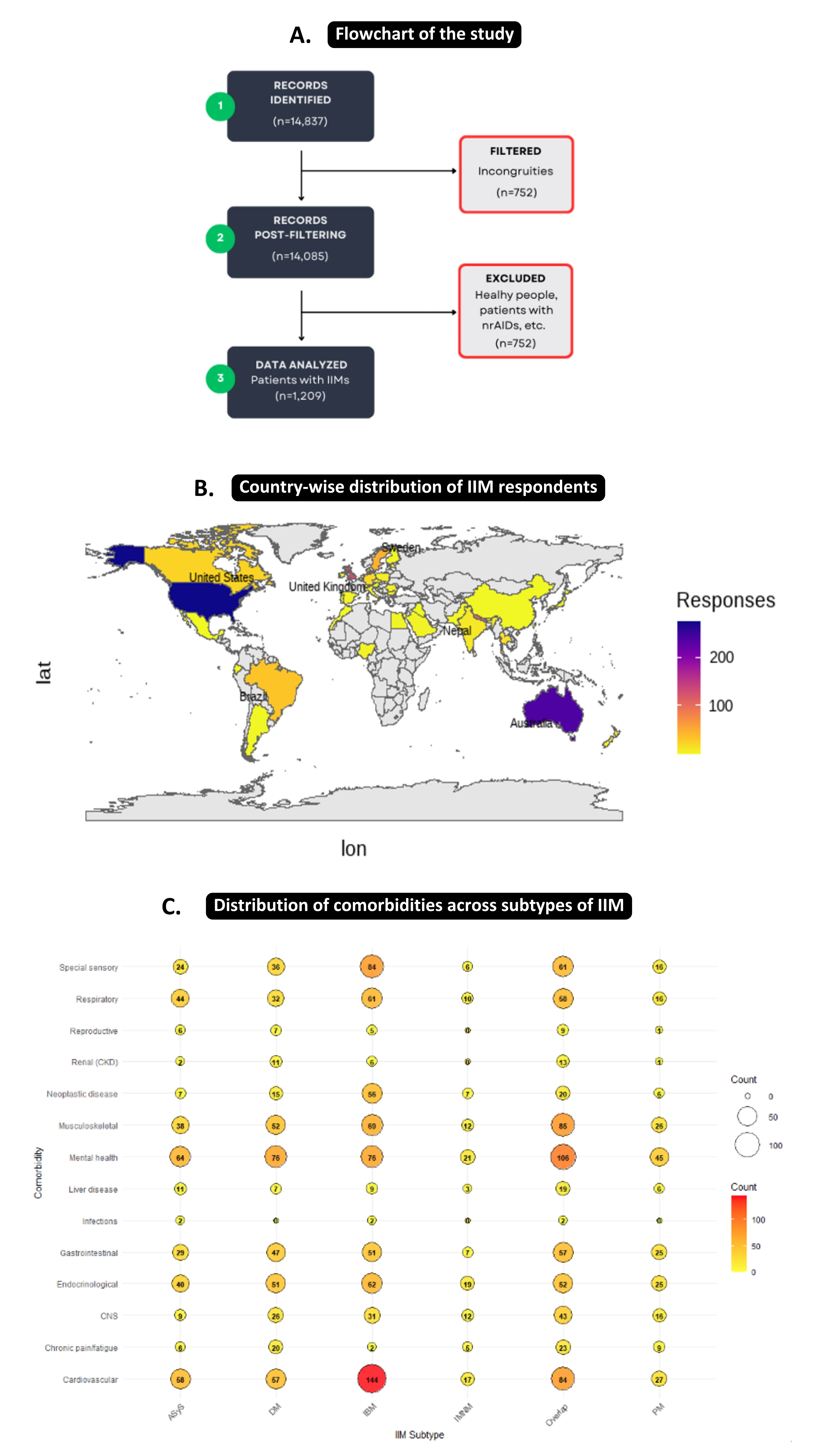 Fig.1: A- Flowchart depicting inclusion of participants; B- World map showing country-wise distribution of IIM respondents; C- Distribution of comorbidities across IIM subtypes
Fig.1: A- Flowchart depicting inclusion of participants; B- World map showing country-wise distribution of IIM respondents; C- Distribution of comorbidities across IIM subtypes
.jpg) Fig.2: A- Hierarchical cluster analysis in IIMs; B- Distribution of IIM subtypes in different clusters
Fig.2: A- Hierarchical cluster analysis in IIMs; B- Distribution of IIM subtypes in different clusters
.jpg) Table 1: Characteristics of study sample
Table 1: Characteristics of study sample
To cite this abstract in AMA style:
Coskun Benlidayi I, Lama M, Afolayan O, Shah M, Sarkar M, Rubinstein T, Opinc-Rosiak A, Miskovic R, Milchert M, Luz Felipe da Silva D, Shinjo S, Nikiphorou E, Parodis I, Venerito V, Agarwal V, Gupta L. Patterns of Comorbidity in Idiopathic Inflammatory Myopathies: A Cross-sectional Analysis of Disease Burden and Risk Factors [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/patterns-of-comorbidity-in-idiopathic-inflammatory-myopathies-a-cross-sectional-analysis-of-disease-burden-and-risk-factors/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patterns-of-comorbidity-in-idiopathic-inflammatory-myopathies-a-cross-sectional-analysis-of-disease-burden-and-risk-factors/
