Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The risk of severe acute COVID-19 infection has substantially decreased since the start of the pandemic. However, the risk of severe acute COVID-19 outcomes in the recent Omicron era among individuals with systemic autoimmune rheumatic diseases (SARDs) has not been well studied. We evaluated the risk of hospitalization due to COVID-19 as well as factors associated with increased odds of hospitalization.
Methods: We identified patients with SARDs and COVID-19 infection from September 1, 2022, when the first SARS-CoV-2 bivalent vaccine became available, through March 15, 2024 in a large US healthcare system. Individuals were identified from positive tests or COVID-19 antiviral prescription in the EHR, and/or by patient report of a positive home test to their physician, and COVID-19 infection was confirmed by chart review. Each patient’s first COVID-19 infection within the study period was considered. The primary outcome was hospitalization due to COVID-19 infection, as determined by a physician investigator, within 30 days of COVID-19 diagnosis. We also evaluated days of hospitalization, level of care required, and death within 90 days of infection. We estimated the associations of baseline characteristics with the odds of hospitalization for COVID-19 infection using multivariable logistic regression.
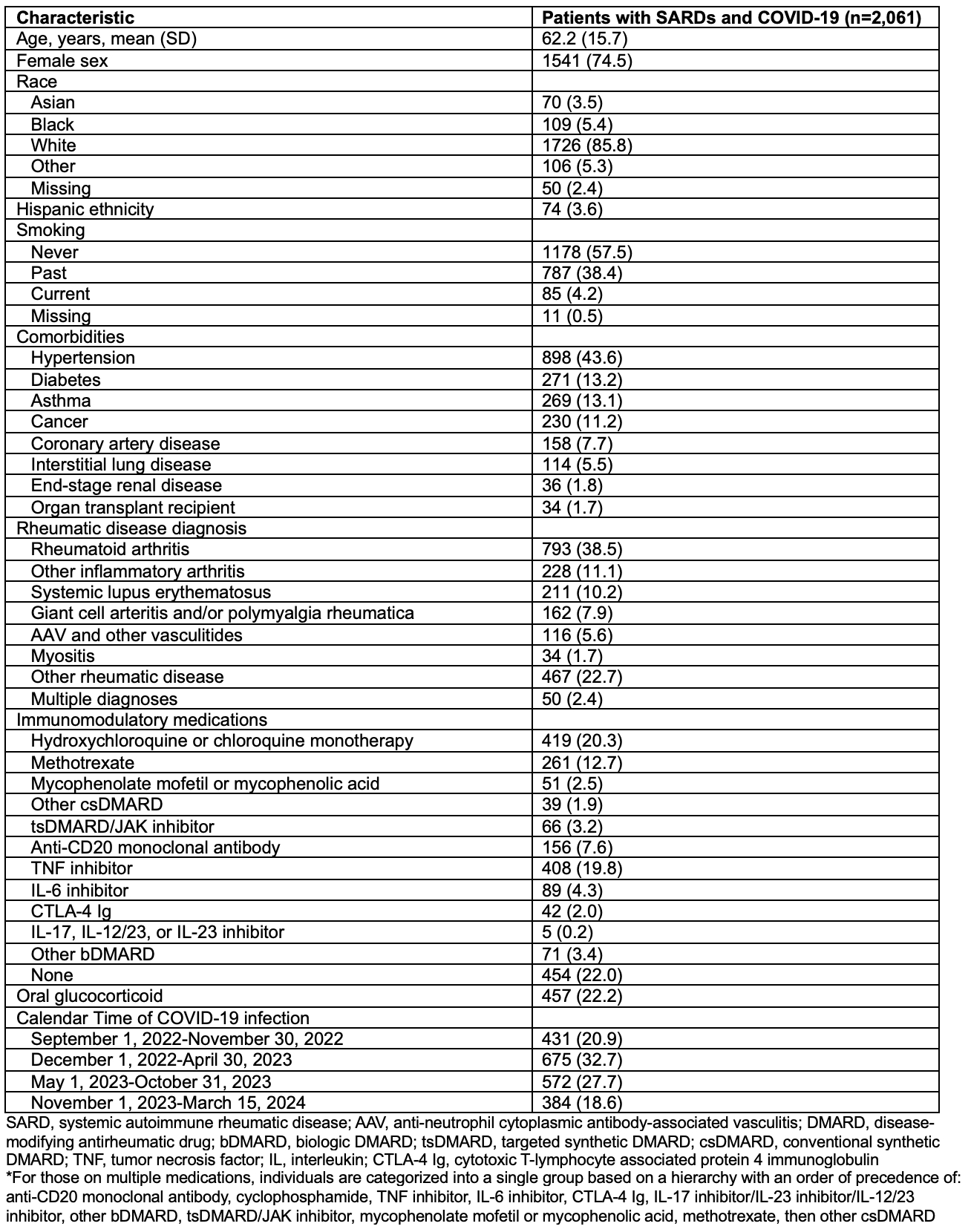
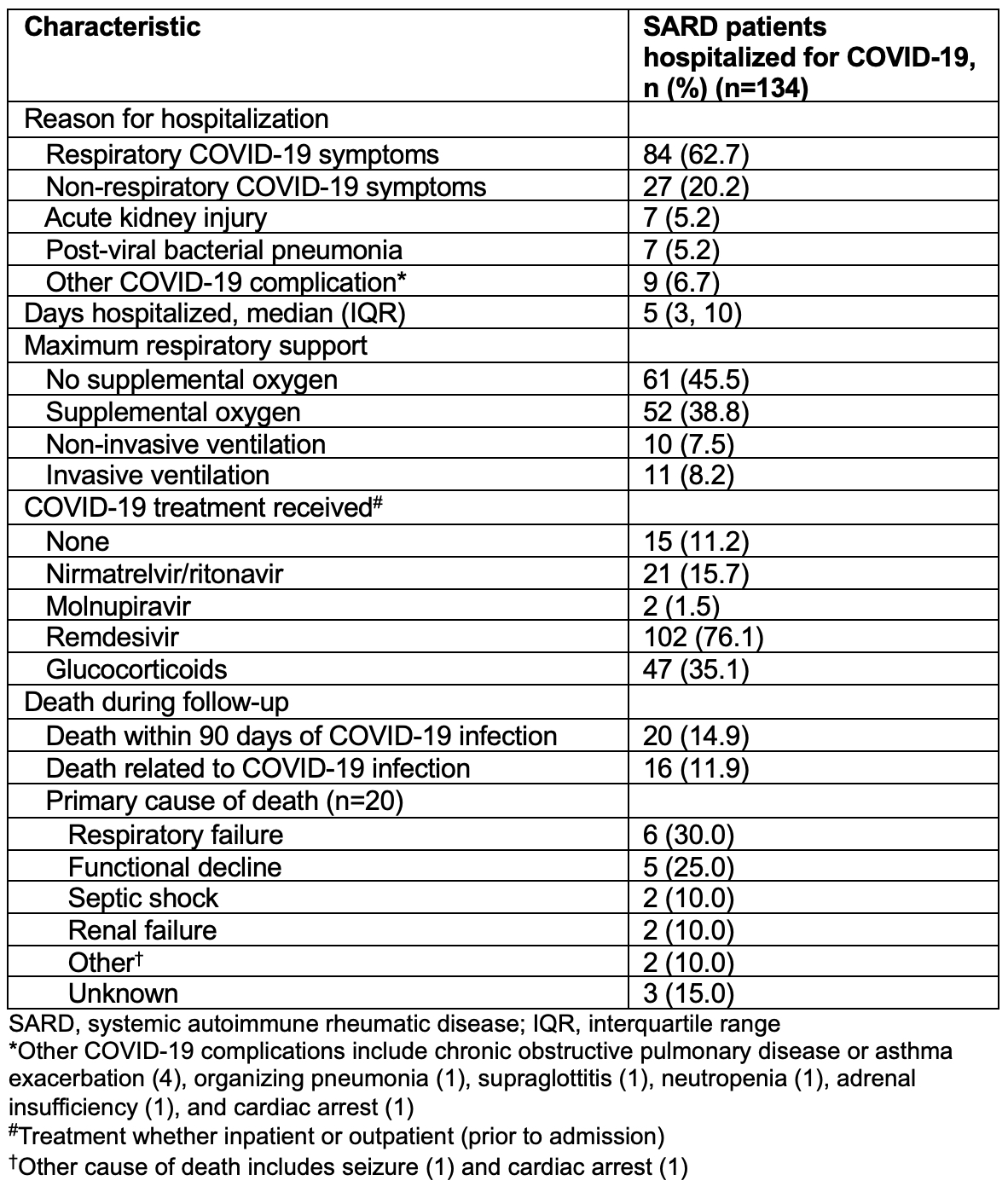
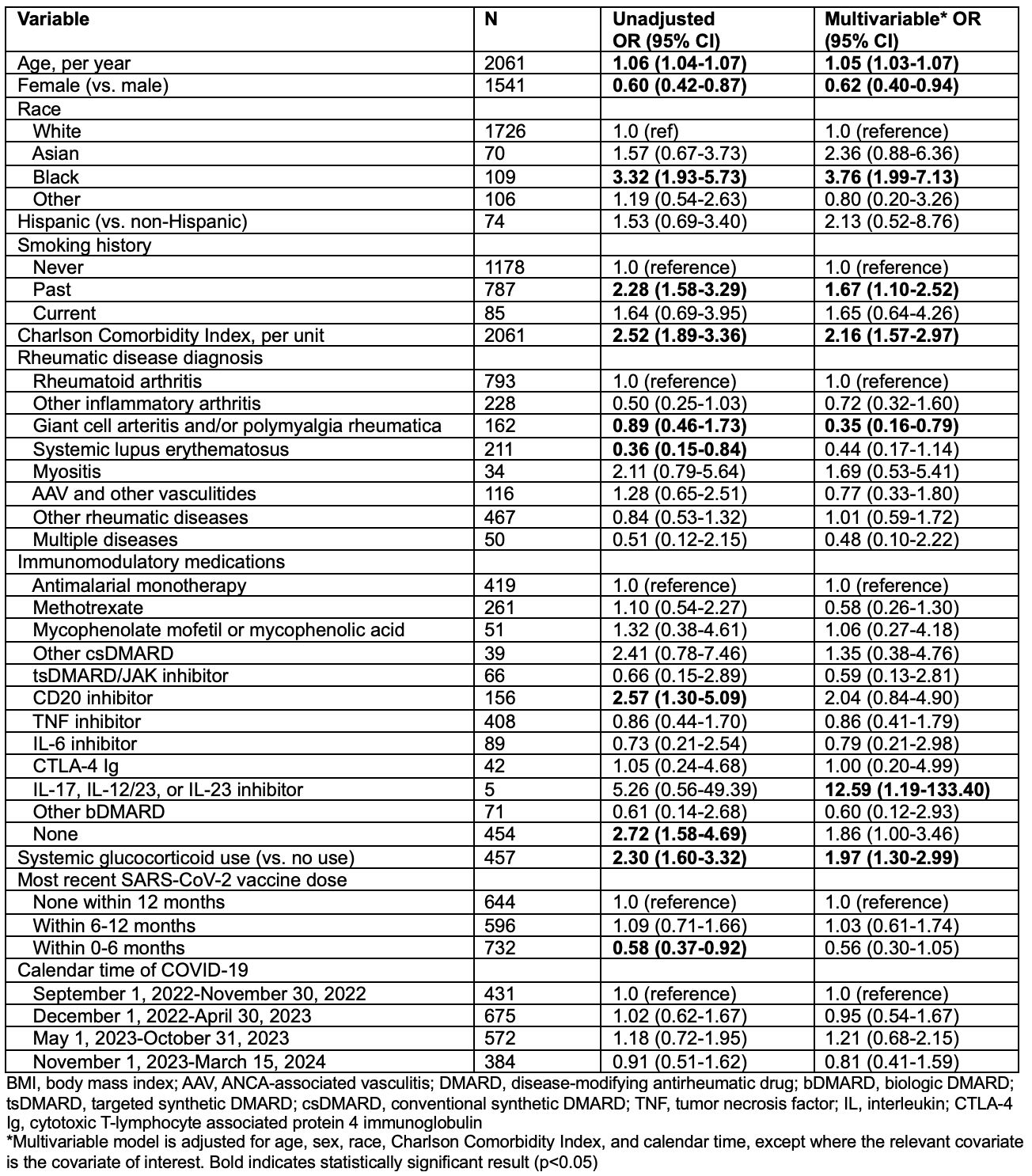
Results: Among 2,061 patients (75% female, mean age 62.2 years) (Table 1), 134 (6.5%) were hospitalized due to COVID-19 infection. Of these, COVID-19 respiratory symptoms were the most common reason for hospitalization (63%), followed by non-respiratory COVID-19 symptoms (20%) (Table 2). Of those hospitalized, 39% required supplemental oxygen, 8% required non-invasive ventilation, 8% required mechanical ventilation, and 20 (15%) died within 90 days of COVID-19 infection. Age (adjusted odds ratio [aOR] 1.05 per year), Black race (aOR 3.76, vs. White race), higher Charlson Comorbidity Index (aOR 2.16 per unit), and past smoking (aOR 1.67, vs. never smoking) were associated with higher odds of hospitalization (Table 3). Female sex (aOR 0.62, vs. male sex) and diagnosis of GCA and/or PMR (aOR 0.35, vs. RA) were associated with lower odds of hospitalization. Compared to those on antimalarial monotherapy, those on CD20 inhibitors had numerically higher odds of hospitalization (aOR 2.04). Those on IL-17, 12/23, or 23 inhibitors had higher odds of hospitalization (aOR 12.59) though this subgroup only contained 5 individuals. Systemic glucocorticoid use was associated with higher odds of hospitalization (aOR 1.97, vs. non-use). There was a trend toward lower odds of hospitalization with a SARS-CoV-2 vaccine in the past 0-6 months (aOR 0.58 vs. no vaccine within 12 months). There was no association of calendar time within the study period with hospitalization for COVID-19.
Conclusion: Patients with SARDs remain at risk of hospitalization for COVID-19, even in the contemporary Omicron era. Risk factors for hospitalization include older age, Black race, greater comorbidity burden, and systemic glucocorticoid use. Ongoing mitigation measures including updated vaccinations and pre-exposure prophylaxis should be utilized as recommended.
To cite this abstract in AMA style:
Patel N, King A, Srivatsan S, Wang X, Kowalski E, Vanni K, Qian G, Hanberg J, Bade K, Saavedra A, Mueller K, Williams Z, Johnson C, Negron M, Sparks J, Wallace Z. Patients with Systemic Autoimmune Rheumatic Diseases Remain at Risk for Hospitalization for COVID-19 Infection in the Omicron Era (2022-2024): A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/patients-with-systemic-autoimmune-rheumatic-diseases-remain-at-risk-for-hospitalization-for-covid-19-infection-in-the-omicron-era-2022-2024-a-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patients-with-systemic-autoimmune-rheumatic-diseases-remain-at-risk-for-hospitalization-for-covid-19-infection-in-the-omicron-era-2022-2024-a-retrospective-cohort-study/