Session Information
Date: Monday, November 13, 2023
Title: (1013–1032) Healthcare Disparities in Rheumatology Poster II: Socioeconomic Determinants
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: While racial/ethnic disparities in total joint arthroplasty (TJA) utilization are well-documented, the impact of orthopedic specialists on patients’ perceptions of TJA is poorly understood. We aimed to assess the relationship between orthopedic consultation and patients’ perspectives on TJA barriers.
Methods: This multi-institutional prospective cohort study was conducted from 2/2020 to 7/2022. We surveyed patients at 2 large urban academic institutions (Hospital for Special Surgery; New York Presbyterian-Brooklyn Methodist Hospital) and 2 national arthritis cohorts (ArthritisPower; CreakyJoints Español). The electronic questionnaire was developed through thematic analysis of semi-structured interviews conducted with minority patients experiencing advanced osteoarthritis. The questionnaire assessed participants’ barriers to TJA were using a 5-level Likert scale. Responses were categorized through a top-2 box analysis: “Highly important” (very or extremely important) and “Not as important” (bottom 3 levels). We evaluated differences in characteristics between those who had and those who had not consulted an orthopedist. Multiple logistic regression models were used to analyze the adjusted odds ratios (aOR) of orthopedic consultation on patients’ ratings of barriers to TJA. Models controlled for patient factors, including race, age, HOOS, JR/KOOS, JR, insurance, education, and prior discussion of TJA with any doctor.
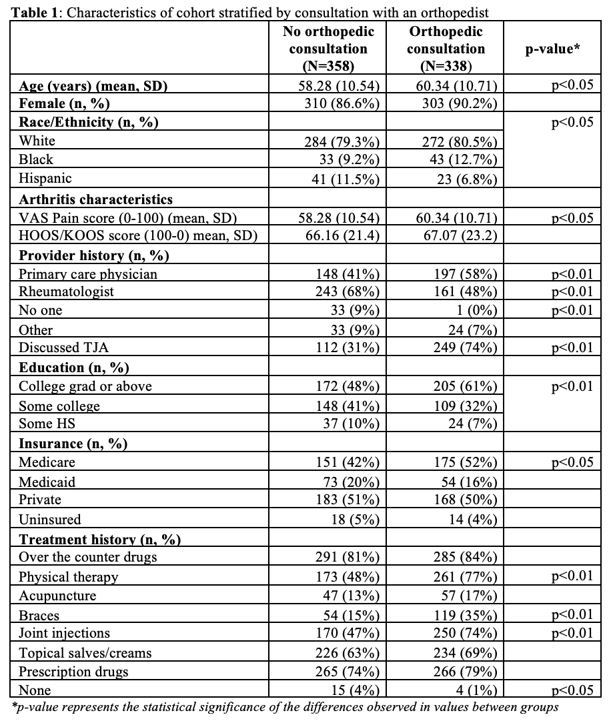
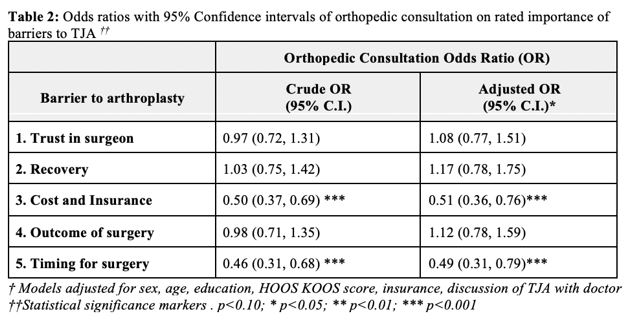
Results: 696 participants who completed the survey were included in the analysis (94% of respondents; 24% of total queried). Most were female (88%), average age 59.3 years, 77% White participants, 11% Black, and 9% Hispanic. 49% reported having had an orthopedic consultation. The questionnaire examined five TJA barriers: 1. Trust in surgeon, including factors like finding a qualified surgeon; 2. Cost/insurance, such as challenges related to co-pays and insurance coverage; 3. Recovery concerns, such as insufficient social support; 4. Surgical outcome, such as the potential need for additional TJA due to young age; and 5. Timing of surgery, whereby other health concerns take precedence over TJA. Participants who had consulted with an orthopedist were older (p< 0.05), more likely to be college graduates (p< 0.01), Medicare beneficiaries (p< 0.05), have consulted with a primary care physician (p< 0.01), and have attempted arthritis treatments, such as joint injections (p< 0.01), braces (p< 0.01), and physical therapy (p< 0.01) (Table 1). After adjusting for patient factors, orthopedic consultation was a significant predictor of lower barriers relating to cost/insurance (aOR (95% CI): 0.52 (0.36, 0.76)) and timing of surgery (aOR (95% CI): 0.49 (0.31, 0.79)). (Table 2) Patient factors, including race and insurance, did not have significant interaction with orthopedic consultation (all p >0.05).
Conclusion: While those with an orthopedic consultation were able to overcome cost/insurance and timing barriers to consider TJA, significant barriers persisted. Developing strategies to identify and address the TJA barriers among minority groups may help increase utilization within these groups.
To cite this abstract in AMA style:
Mannstadt I, Gibbons J, Amen T, Rajan M, Young S, Parks M, Figgie M, Bass A, Russell L, Mehta B, Navarro-Millán i, Goodman S. Patients’ Barriers to Total Joint Arthroplasty: Associations with the Orthopedic Consultation [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/patients-barriers-to-total-joint-arthroplasty-associations-with-the-orthopedic-consultation/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patients-barriers-to-total-joint-arthroplasty-associations-with-the-orthopedic-consultation/