Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: In clinical practice, it is often challenging to distinguish fibromyalgia syndrome (FMS) from axial spondyloarthritis (axSpA), which includes ankylosing spondylitis and non-radiographic axSpA. Early stages of axSpA may present with an onset similar to FMS, and likewise patients with FMS may have symptoms that are similar to axSpA. Differentiating between axSpA and FMS can also be challenging for patients and can cause confusion about their diagnosis. This study examined the prevalence of axSpA symptoms among patients with FMS and differences in the pathway to diagnosis among patients with and without concomitant axSpA.
Methods: Adult US patients with FMS without concomitant rheumatoid arthritis or psoriatic arthritis in the ArthritisPower registry received email invitations to participate. Participants (pts) were asked whether they had a diagnosis of axSpA or ankylosing spondylitis and completed patient-reported outcome measures including Patient Reported Outcomes Measurement Information System (PROMIS) measures for Pain Interference, Sleep Disturbance and Fatigue, and the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). Pts then responded to a 57-item customized survey developed by the researchers in collaboration with patient partners. Results are descriptively reported.
Results: As of March 2020, 301 pts completed the survey; 97% female, 90% White, mean (SD) age of 53 (10). Mean (SD) Pain Interference score was 68 (5); Sleep Disturbance 64 (8); Fatigue 69 (6); and BASDAI 46 (8). Of the pts, 44 (15%) reported concomitant axSpA, 61% osteoarthritis, 6% gout, 5% Crohn’s or ulcerative colitis, and 4% lupus. Half (52%) of all pts perceived their FMS to be ‘rarely’ or ‘never’ well managed and 80% ever felt that they have had an additional undiagnosed condition. Three-fourths (74%) of pts reported being able to differentiate between their FMS pain and pain from a concomitant disorder. Back pain lasting >3 months was reported by 93% of axSpA pts and 94% of non-axSpA pts; 11% reported all of the symptoms consistent with patient reported versions of the Assessment of SpondyloArthritis International Society (ASAS) criteria (back/buttock pain >3 months; age of symptom onset < 45; sacroiliitis diagnosis; at least one spondyloarthritis feature) (Figure 1), and of these, 32% reported an axSpA diagnosis. More pts with axSpA received their FMS diagnosis by a rheumatologist (45%) than without (41%) (Figure 2). Of the pts without an axSpA diagnosis (n=257), only 7% recalled their provider ever discussing with them the possibility of axSpA, including non-radiographic axSpA. Half (52%) of pts with axSpA believe that their axSpA should have been diagnosed earlier, with 39% reporting one reason for the delay as their doctors’ belief that FMS was the cause of any axSpA symptoms.
Conclusion: Patients with FMS often experience symptoms of axSpA and the two conditions can occur concomitantly. Additional research is needed to improve the triage, diagnosis, and education of patients with FMS and symptoms of axSpA.
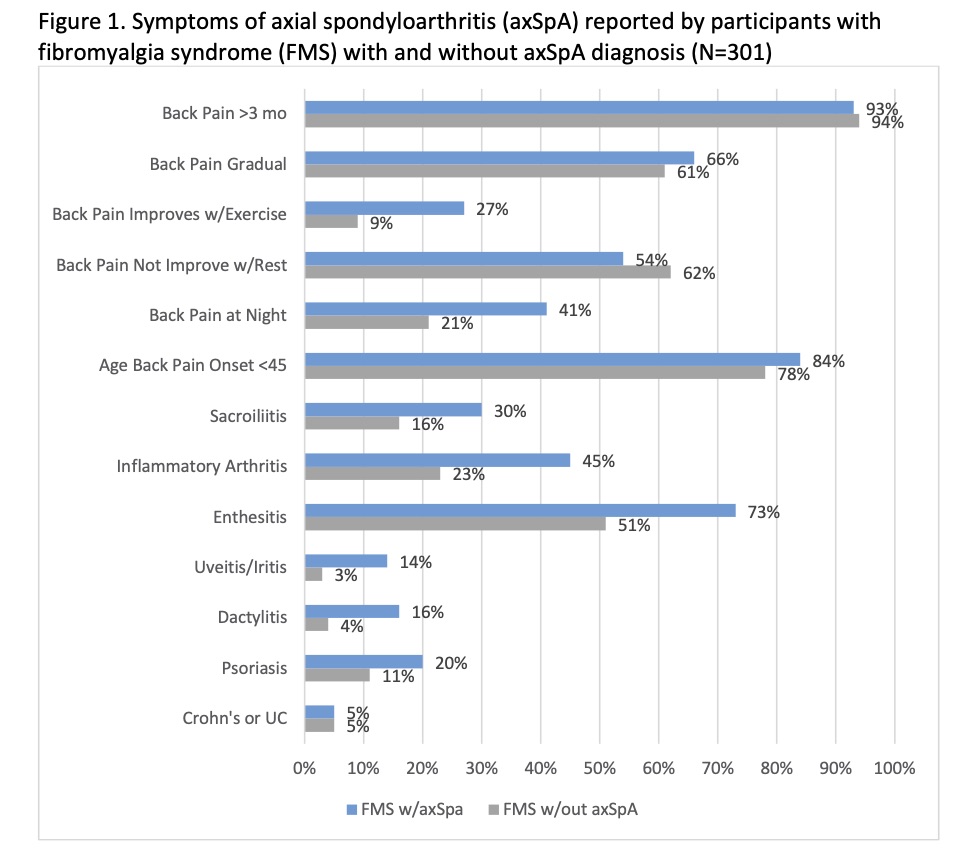 Figure 1. Symptoms of axial spondyloarthritis (axSpA) reported by participants with fibromyalgia syndrome (FMS) with and without axSpA diagnosis (N=301)
Figure 1. Symptoms of axial spondyloarthritis (axSpA) reported by participants with fibromyalgia syndrome (FMS) with and without axSpA diagnosis (N=301)
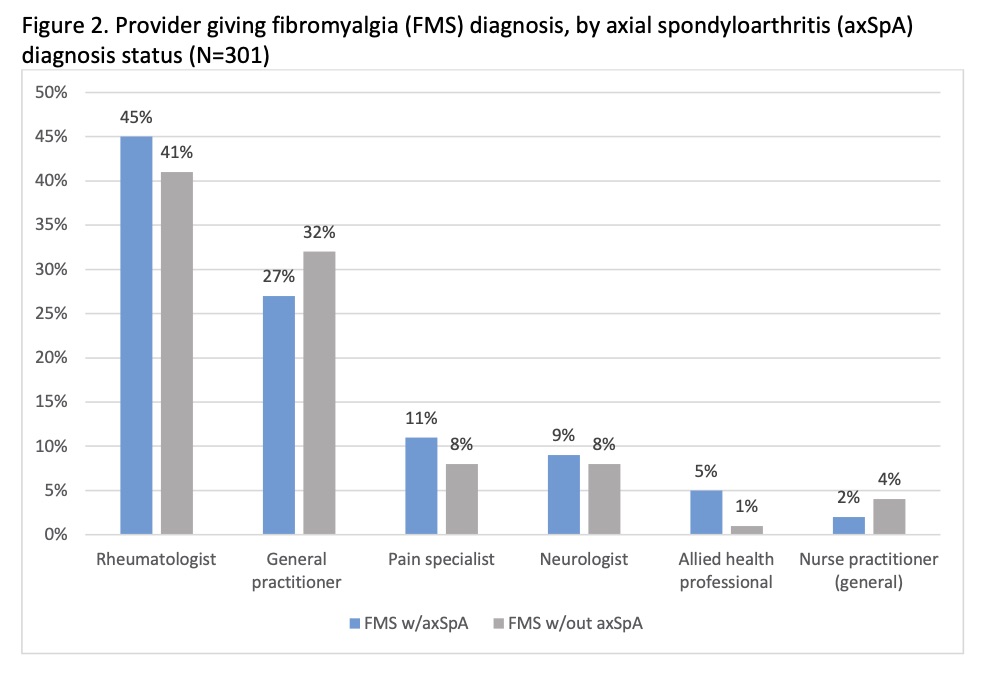 Figure 2. Provider giving fibromyalgia (FMS) diagnosis, by axial spondyloarthritis (axSpA) diagnosis status (N=301)
Figure 2. Provider giving fibromyalgia (FMS) diagnosis, by axial spondyloarthritis (axSpA) diagnosis status (N=301)
To cite this abstract in AMA style:
Gavigan K, Nowell W, Reynolds R, Stradford L, Curtis J, Ogdie A. Patient Perceptions of Fibromyalgia Symptoms and the Overlap with Axial Spondyloarthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/patient-perceptions-of-fibromyalgia-symptoms-and-the-overlap-with-axial-spondyloarthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-perceptions-of-fibromyalgia-symptoms-and-the-overlap-with-axial-spondyloarthritis/
